When the “Triple Aim” was developed in 2007, the focus was threefold: improved patient experience, better outcomes, and lower costs. The 2014 update made it a “Quadruple Aim” with the addition of workforce well-being. Most recently, in 2021, just as health disparities were being illuminated by the COVID-19 pandemic, the explicit goal of health equity was added, creating the “Quintuple Aim”.

In terms of prior authorization, compliance with federal and state legislation is essential, but when health plans look at prior authorization through the lens of the Quintuple Aim, the process demands more. Health plans will need to consider individual service and procedure requests from a broader context if they want to achieve administrative cost and medical expense savings while promoting equitable, high-quality patient care. In addition to ensuring that patients receive the right care, at the right time, in the right setting, the Quintuple Aim reminds those of us who work in case management to ensure that patients’ unique needs, preferences, and values are taken into consideration throughout the prior authorization and/or utilization management process. An ideal state also brings social drivers, or determinants, of health (SDOH) into view. One SDOH example which comes to mind is a patient’s access to transportation. Even if a prior authorization request for a scheduled procedure is approved, the patient will not get the care they need if they do not have transportation to the procedure.
Prior authorization within a value-based care context shifts the focus away from the individual costs of tests and procedures and instead, reframes the services within the context of the patient’s unique care journey, from clinical presentation to desired outcome(s). Because the physicians’ reimbursement amounts depend, in part, on meeting quality and patient experience measures, the entire practice is focused on improving quality. With the technological advances of intelligent prior authorization, it is possible to align utilization review to achieve end-to-end, value-based care. Some examples of this innovative approach are the alignment of services within evidence-based care paths, the use of proactive moments of influence, and bundling related authorization requests into an episodic authorization.
Drawing from the data gathered from the authorization requests themselves and analyzing the claims data for patient cohorts with similar diagnoses and circumstances, intelligent prior authorization solutions align a service request within an evidence-based care pathway. Policy-agnostic and aligned with clinical guidelines, these data-driven care paths allow for a more patient-centered approach when considering a service request, transforming utilization review from transactional to longitudinal.
Patient cohorting and care paths can also be used to promote high-value care earlier, or further upstream, in a patient’s journey. For example, intelligent prior authorization solutions can leverage health plan data combined with additional clinical information to nudge toward the most appropriate, high-value care. Clinical nudges can be deployed to suggest an alternative service or site of care to enable auto-determining or take advantage of moments of influence to suggest lower-cost, evidence-based, and possibly underutilized services that the physician might not have on their radar.
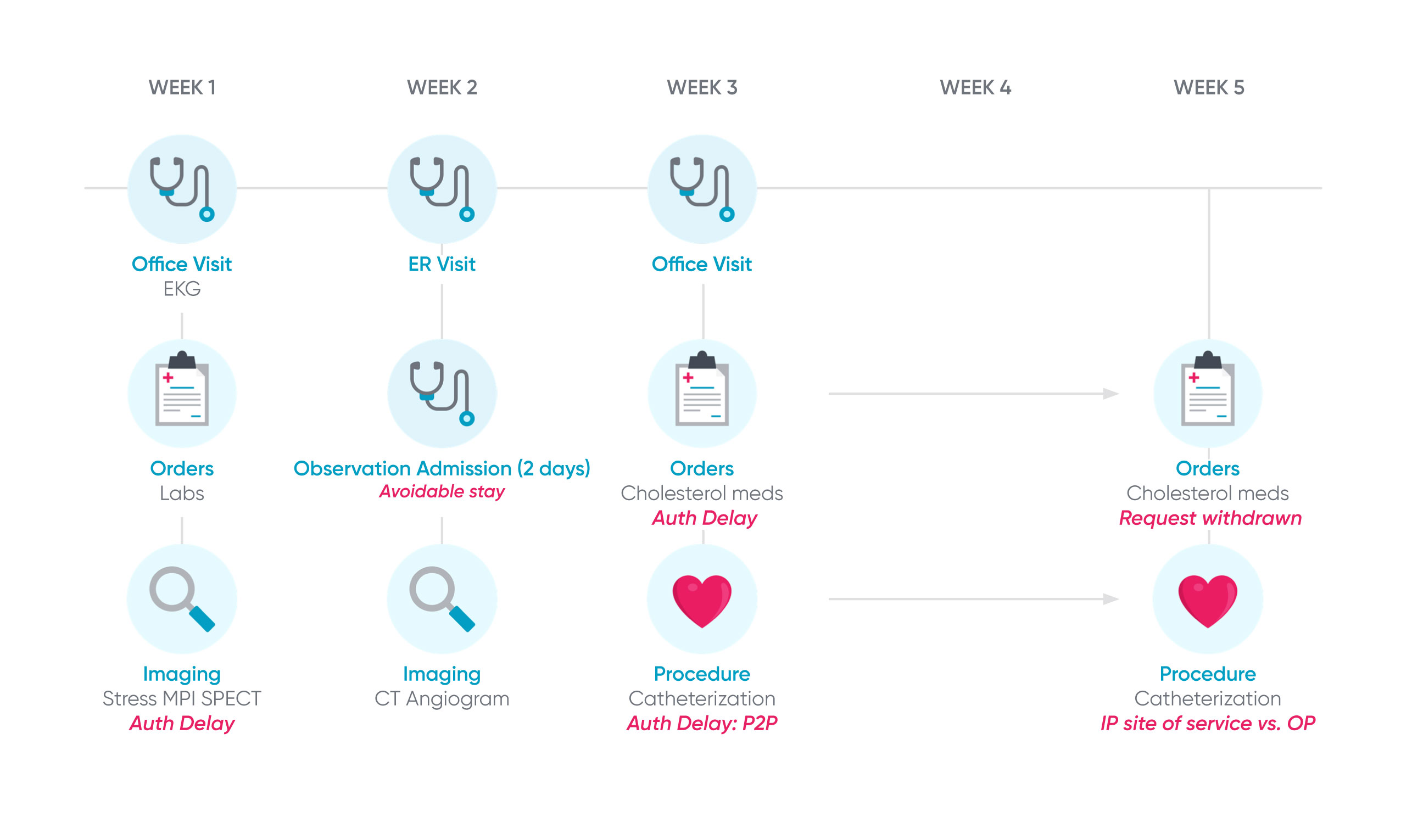
Consider the patient example below: Hazel Corcoran visits her cardiologist after experiencing chest pain. He administers an EKG, but wants Hazel to get an MPI SPECT. However, because of prior authorization delays, Hazel gets frustrated and goes to the ER. The ER doctor orders a CT angiogram and then admits her for two days for observation. After her discharge, she sees her cardiologist again, who prescribes a new cholesterol medication and wants Hazel to undergo a cardiac catheterization, both of which require prior authorization. The catheterization approval ends up requiring a peer-to-peer, delaying the process by two weeks. When the catheterization is approved, Hazel undergoes the outpatient procedure at the hospital. This patient journey takes about 33 days.
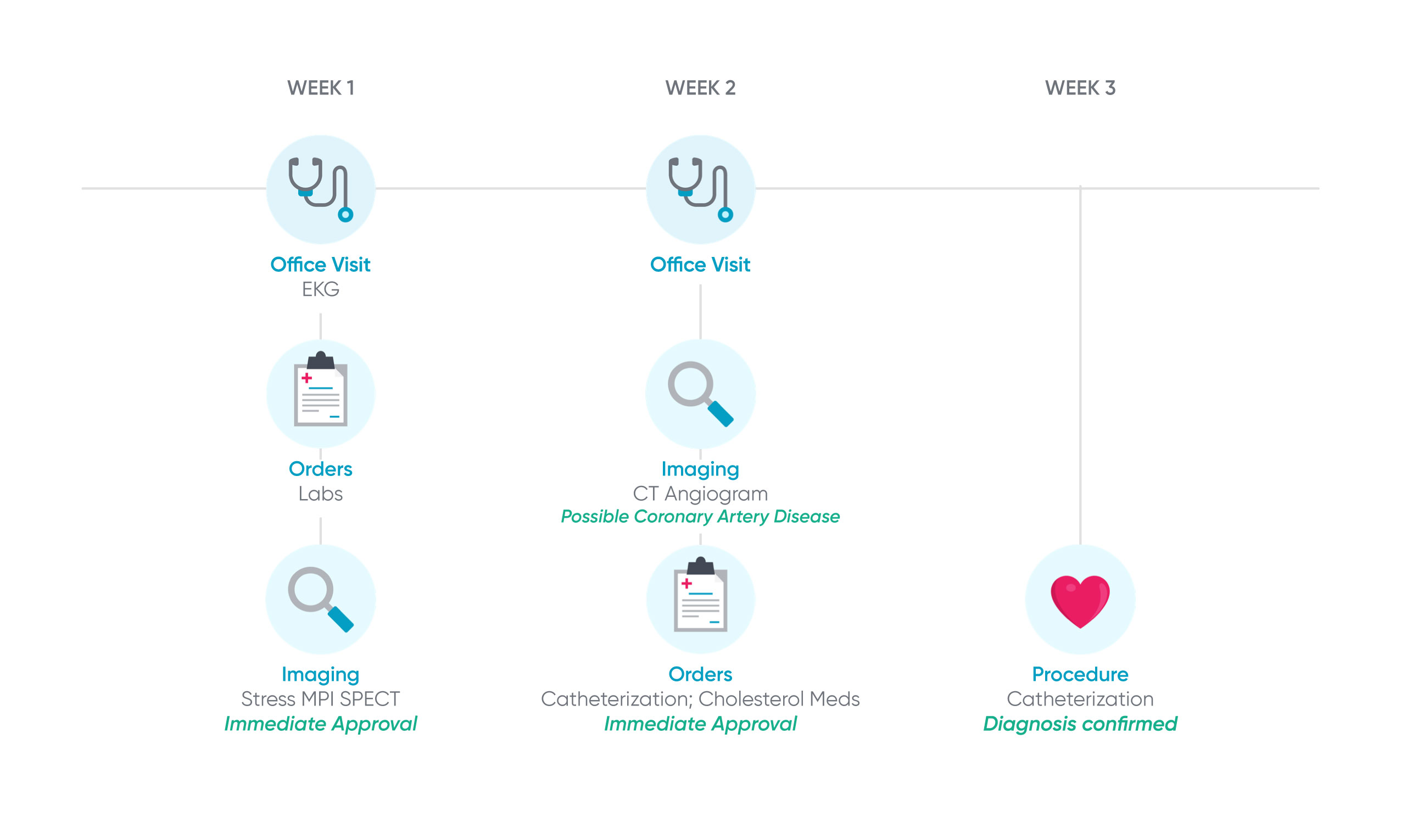
Intelligent prior authorization solutions align the authorization requests on an evidence-based care path and deploys nudges to reduce variations in care and shorten the patient journey. The figure below shows Hazel’s patient journey with intelligent prior authorization.
Hazel visits a cardiologist for her chest pain, where she receives an exam and EKG. The cardiologist checks her cholesterol and orders a stress MPI SPECT. Because the cardiologist submits a prior authorization for the MPI SPECT using intelligent prior authorization, it is automatically approved. Hazel receives the CT angiogram, which shows possible coronary artery disease. This timely diagnosis enables a quicker path to treatment and therefore, Hazel doesn’t go to the ER for an unnecessary visit because she is frustrated. When Hazel next visits her cardiologist, she is prescribed new cholesterol medication and ordered a catheterization, for which the prior authorizations for both are automatically approved. Drawing from patient cohorting data, a clinical nudge informed the requesting provider that the site-of-service for this procedure could be appropriately shifted to an outpatient setting to reduce cost. This resulting patient journey takes only 15 days, enhancing provider and patient experience, and delivering cost savings for the health plan.
Intelligent prior authorization harnesses artificial intelligence (AI) and machine learning to suggest related services and aggregate them into a single “episodic authorization” request, shortening the timeline for access to care, and helping to place a service within the context of patient care journey. Authorizations oriented around an entire care journey instead of a single service introduce a more comprehensive and equitable approach to utilization management.
Health plans should look to the quintuple aim instead of just regulatory compliance.
Health plans should use intelligent prior authorization as a way to not only comply with the changing landscape of healthcare, but to use its advanced capabilities to leverage patient, physician, and regional population data to orient prior authorizations to the patient care journey, aligning with value-based models.
Intelligent prior authorization connects the dots between electronic prior authorization and the doors opened by the data that exists from its digitization. While legacy approaches to prior authorization solve some of the issues, like physician burden and patient access to care, intelligent prior authorization takes it to the next level. This transformative approach reimagines the utilization management process to align health plans and providers toward driving better value for patients, and has the power to help ensure equitable care.
To learn more about intelligent prior authorization, download our white paper.

