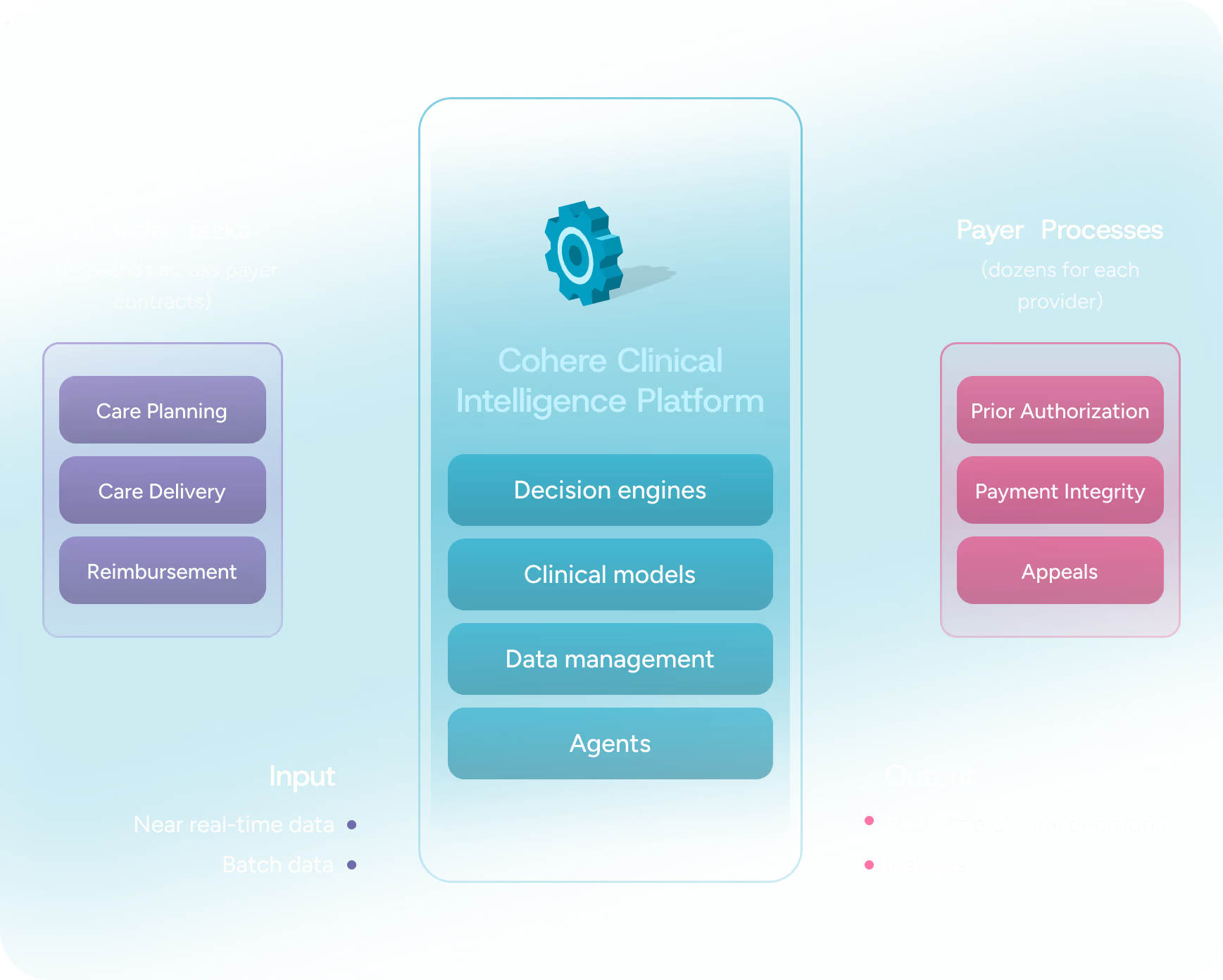
Why Cohere Health®?
Choose a clinical intelligence platform that proactively solves your enterprise challenges
Cohere's clinical intelligence platform equips health plans with AI-driven actionable insights that go far beyond traditional utilization management systems, legacy portals and vendors, and outdated cost containment operations, powering decisions on care quality, utilization, and care value.