Increasing the use of advanced technology applications in the prior authorization process helps health plans reduce physician burden and improve quality of patient care. As health plans and other stakeholders get more comfortable with AI, it can drive true transformation in utilization management, as the five trends below demonstrate.
1. Vintage can still be modern
Utilization management and prior authorization specifically, is facing much criticism for its time-consuming and inefficient processes that create an undue burden for providers and can delay care for patients. Recent regulations, both final and proposed rules, from The Centers for Medicare and Medicaid (CMS) focus on digitizing the process to minimize the effects of prior authorization on disadvantaged patient populations.
However, these regulations only focus on one side of the process: the part controlled by health plans. Smaller practices and health systems might not be able to quickly adopt digital prior authorization processes.
Intelligent prior authorization meets health plans and providers where they are while improving the process for everyone and laying the foundation for more advanced AI-driven capabilities. Optical character recognition (OCR) and machine learning (ML) technology digitize manual inputs, like faxed prior authorization requests, to enable automated utilization review while keeping the process unchanged for providers unable to adjust as quickly. Health plans can achieve regulatory compliance and improve administrative efficiencies without increasing the burden on providers unable to make the change.
2. The year of yes
Advancements enabled by prior authorization digitization don’t end there, for providers and health plans open to the possibilities. FHIR-based APIs digitize and improve transparency between providers and health plans, and make it possible to automate the decisioning of prior authorization requests. Here’s what’s possible:
-
- Eliminate review of unnecessary prior authorization submissions by automatically determining if an authorization is required, before submitting one, saving administrative time and expense.
- Automatically send provider notifications of missing information using machine learning and OCR models to identify and recognize critical clinical evidence and alert providers if it is missing to reduce manual outreach.
- Automate clinical review for 50-80% of cases, depending on specialty, using a combination of coverage requirements discovery (CRD), documentation, templates, and rules (DTR), and prior authorization support (PAS) APIs, freeing clinical reviewers to focus their attention on the fewer complex cases requiring manual review.
- Accelerate manual review with pre-process documentation by using machine learning models trained in healthcare data to scan clinical documentation and lighten the administrative burden on clinical reviewers.
3. A nudge in the right direction
Prior authorization’s administrative burden is so pronounced that 35% of providers employ staff just to work on prior authorization alone. With so many requests submitted by administrators without medical backgrounds, it is not surprising that requests may be incomplete (missing necessary information) and inaccurate (duplicate requests show different answers to clinical questions answered in the previous submission).
Health plans can improve the accuracy of prior authorizations, saving administrative and medical expense, by reducing reliance on user-submitted information, like clinical assessment questionnaires (CAQs). For example, AI can extract relevant clinical data directly from clinical notes, or can mine claims history for previous iterations of that service.
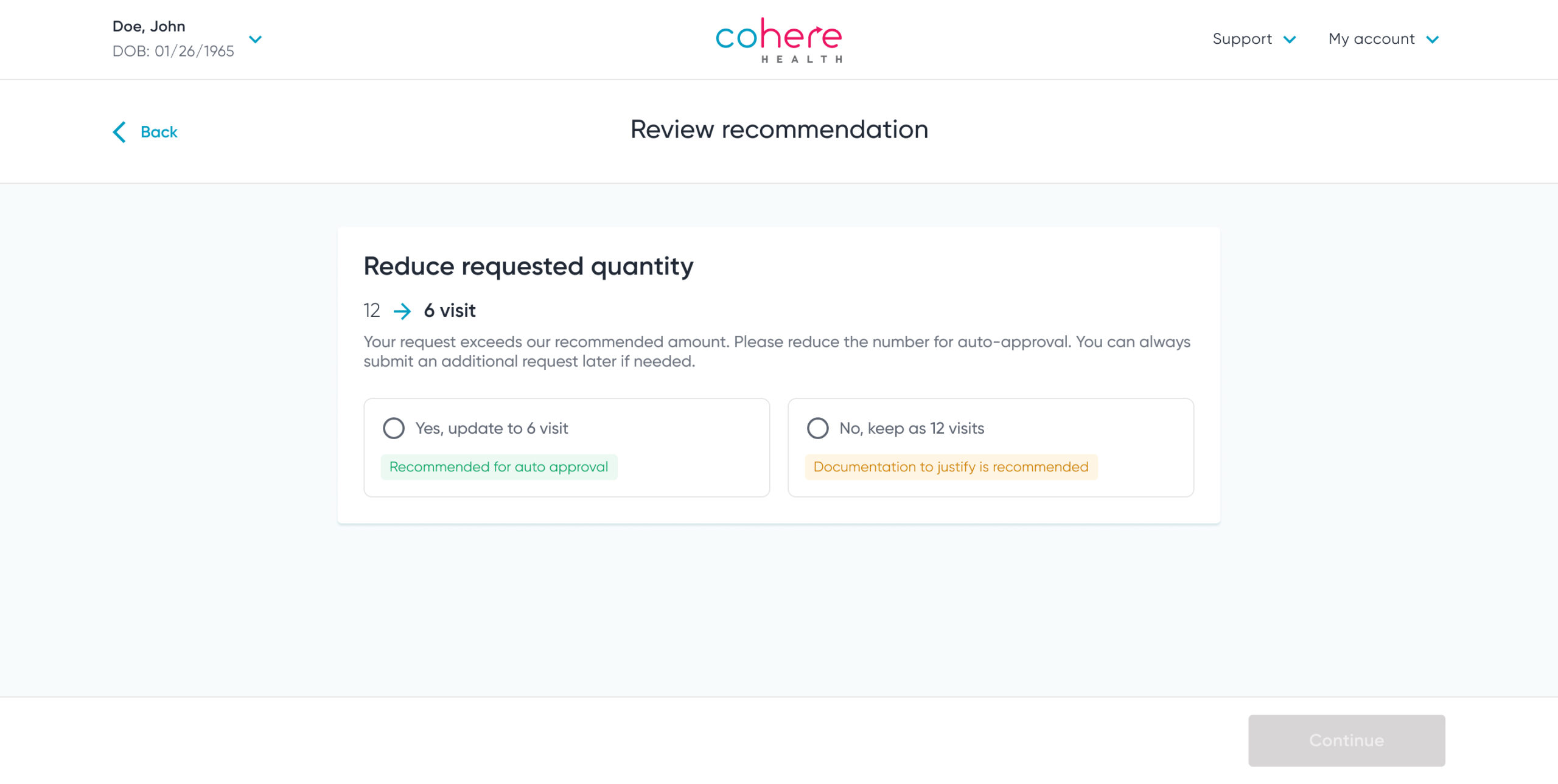
Once this information is uncovered from these large data sets, health plans can leverage the prior authorization transaction as an opportunity to improve care quality by surfacing this information to providers in the form of an in-workflow notification called a nudge. For example, if a provider requests more than the number of physical therapy visits allowed by health plan policy, the provider would receive a notification alerting them of this and asking if they would consider adjusting the number to receive an automatic, instant approval.
4. Getting the green light
Despite state-level legislative support, gold carding programs are so difficult to implement that many health plans have discontinued their (voluntary) programs, citing the following reasons:
-
- It was administratively difficult to implement – 75%
- It reduced quality and/or patient safety – 50%
- It increased costs without improving quality –25
Intelligent prior authorization’s green lighting programs offer a compliant alternative to gold carding without removing patient safety and overutilization safeguards. Green lighting leverages a prior notification system that reduces the administrative burden for high-value providers. The program identifies eligible providers using continuous provider- and service-specific analytics instead of moment-in-time data used by gold carding programs. Health plans can help drive higher-quality patient outcomes through the use of provider-specific, real-time administrative data. For example, by leveraging prior authorization transactions as an opportunity to collaborate with lower-performing providers and improve documentation or care recommendations, health plans can promote greater health equity for patients.
5. Everyone’s an individual
Health plans can go beyond transactional prior authorization. Intelligent prior authorization uses AI to generate treatment plans tailored to individual patients, reflective of their unique clinical situation, medical history, and lifestyle. AI and machine learning models can also chart ideal journeys based on favorable outcomes for patients with similar clinical attributes. Using OCR and machine learning technologies to pull relevant data from clinical attachments, and using machine learning to identify patient clinical evidence directly from electronic medical records (EMR) further support this approach. AI and machine learning can also analyze previous decisioning and claims data to augment yes/no policy-based automated approvals and ensure decisioning accuracy.
Intelligent prior authorization’s advanced technologies encourage the adoption of ideal, patient-specific care pathways built from evidence-based guidelines, plan policies, and patient cohort data pulled from EMR and claims.
-
- Care paths use a combination of data signals and clinical evidence to chart ideal patient journeys
- Episodic authorizations automatically approve related services to encourage the adoption of high-value care
- Clinical nudges synthesize patient context to recommend additional services to promote optimal outcomes
Safe, secure, and trustworthy applications of AI technologies are the building blocks of a transformative utilization management strategy. Starting with the most fundamental of these trends and working to increase the adoption of responsible AI into your health plan’s utilization management strategy will not only save administrative costs, but also improve care access, safety, and quality.
Download our AI Index to read more about how AI is changing healthcare.