A recap of Cohere’s recent webinar with ACAP
The Association for Community Affiliated Plans (ACAP) and Cohere hosted a joint webinar focused on “Utilization Management and Prior Authorization Transformation for Medicaid Plans.” The panel, composed of clinical and product leadership at Cohere Health, unpacked well-known friction points impeding access to care for Medicaid patients.
Review this recap if you missed the live discussion to understand how utilization management solutions can improve the efficiency and efficacy of prior authorization beyond just simple automation. Our expert panel also addressed how prior authorization can be leveraged to address critical gaps in social determinants of health often experienced by Medicaid patients.
Panel participants:
- Brian Covino, MD, FAAOS, Chief Medical Officer
- Gina Kim, Chief Product Officer
- Mary Krebs, MD, FAAFP, Associate Medical Director, Primary Care
- Aimee Bailey, RN, Senior Director of Clinical Programs, Oncology
The webinar recording of the webinar is now available on-demand.
Medicaid plans face a unique set of challenges to utilization management based on the social determinants of health disproportionately likely to face their member populations
Dr. Mary Krebs led a discussion spotlighting the unique utilization management challenges facing Medicaid plans. Some of the main factors include:
- Health equity and social drivers: Such restraints as transportation access, food deserts, isolation, behavioral health challenges, and unsafe environments affect patient access to and efficiency of care
- Insufficient networks: Fewer providers accept Medicaid patients due to reduced reimbursement rates and challenging patient populations
- Value-based care: This structure has great potential to drive better care and is attractive to providers. However, these programs often lack the resources to be effectively administered.
Typical prior authorization processes can be abrasive and can delay needed care
Prior authorization is a necessary process to ensure that providers prescribe the appropriate, evidence-based care to their patients. However, due to the highly manual nature of the process, still largely facilitated by fax, there is a lot of room for improvement. Some of the key inefficiencies of prior authorization include:
- Abrasive and non-collaborative: 88% of physicians report prior authorization as a high or extremely high burden
- Clinical decisions lack specificity: 30% of physicians reported prior authorizations are rarely or never evidence-based
- Costly, manual process: Physicians and staff reportedly spend two days per week on prior authorizations
- Delivers suboptimal care for patients: 93% of physicians report that legacy prior authorization processes lead to delays in patient care
Many providers run into continuity issues when treating Medicaid patients due to social determinants of health such as transportation access or limited provider networks. Digitizing this process and facilitating faster access to care is essential to addressing these issues and better serving Medicaid patients.
Solving inefficiencies for Medicaid patients with uniquely positioned utilization management and digital prior authorization solutions
Dr. Brian Covino and I shared how Cohere Health’s evidence-based and patient-specific utilization management and digital prior authorization solutions are uniquely positioned to solve the inefficiencies that are disproportionately affecting Medicaid patients. Cohere’s technology has been developed to leverage the patient and provider data collected from prior authorizations and compare it to population health data to group patients into cohorts comprehensive of multiple concurrent health factors. The result is a differentiating ability to evaluate prior authorization requests against the backdrop of a specific patient’s history.
Cohere’s delegated specialty solutions take a care path approach. Provider collaboration across the entire care journey is possible by combining health plan prior authorization data, health plan-specific guidelines, and national evidence-based guidelines. The strategic alignment of physicians and health plans around longitudinal care and high-value services has proven successful for patient cohorts and can take social determinants of health into account.
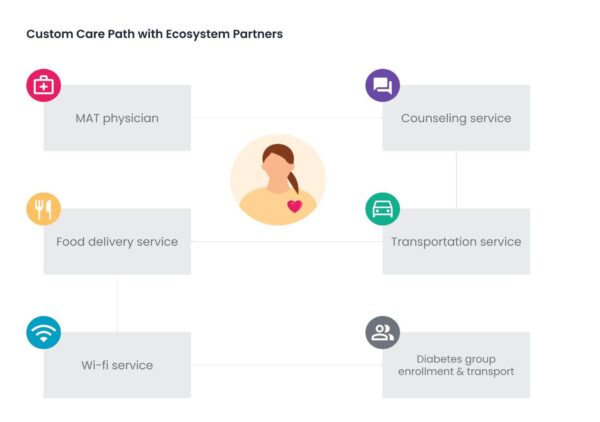
Take, for example, this custom care path created for a patient with diabetes. The care path not only suggests the most appropriate medical services for that specific patient, but also addresses social determinants of health, such as the patient’s poor transportation, isolation, lack of home internet, and placement in a food desert. This strategy can automatically suggest a Medicaid plan’s preferred partners for these services, within the prior authorization workflow, and specific to the patient’s condition and location, thus being more likely to drive better and faster health outcomes.
Nudging toward the future of digital prior authorization
The application of artificial intelligence and machine learning to analyze patient and provider data from health plans to influence providers toward better care choices is referred to as “nudging.” Nudging or nudges are part of Cohere’s approach to transforming utilization management.
Nudges consider the longitudinal patient record and prior authorization data to suggest evidence-based care requests that are more likely to be automatically approved.
These provider nudges result in a faster and higher prior authorization approval rate, as well as driving incremental medical expense savings because, for example, they promote site-of-service programs and route patients to appropriate ecosystem partners.
Ultimately, this downstream and upstream care coordination benefits disadvantaged patient populations affected by social determinants of care.
What do these utilization management innovations mean for plans and patients using Medicaid
The delegated and digital prior authorization solutions discussed during this panel represent a capability to meet providers where they are and deliver end-to-end enhanced provider experience. Through digitizing prior authorization intake across any combination of channels, including digitizing manual or fax submissions, implementation of our portal, or integration with existing EMR systems, Cohere is able to enhance and unify provider experience.
The value is demonstrated by the numbers. Questions during the call indicated an interest in the clinical intelligence expertise woven into this solution and how it is able to accurately automate 90% of prior authorization decisioning. The incremental medical expense is reduced by up to 15%.
By enhancing provider efficiency and experience, Medicaid plans can allow their providers to keep their primary focus on delivering effective care and reduce their administrative burden.
Learn more about how Cohere’s configurable utilization management solutions are best suited to address the unique challenges facing Medicaid plans and to hear the panelists answer questions from the audience, watch the webinar here.