Health plans are caught in a tight financial position. With each year, healthcare costs continue to rise. Patients are already overwhelmed by rising consumer costs and are pressuring their health plans to keep healthcare costs down. However, health plans using intelligent prior authorization leverage early trend signal intelligence to more proactively manage their utilization and mitigate overutilization trends much sooner than with claims-based analysis. By incorporating prior authorization data, which surfaces three months or more earlier than claims-based utilization data, into medical trend forecasting, health plans can more proactively manage both unnecessary costs and medical services.
Did you know that delayed availability of health plan utilization data impedes the ability to influence medical costs?
The rising cost of healthcare is a strain on patients. Half of U.S. adults say it’s difficult to afford healthcare costs, and one in four say they or a family member in their household had problems paying for healthcare in the past 12 months according to a KFF study. Further, four in ten insured adults worry about affording their monthly health insurance premium, and 48% worry about affording their deductible before health insurance kicks in.
Health plans are also feeling the strain: the U.S.’s medical cost trend, the change in the cost to treat patients, has continued its year-over-year increase to 7.0%, up from 6.0% in 2023 and 5.5% in 2022. Health plans want to offer their members the lowest possible premiums but must first ensure that their costs are covered.
One of health plans’ levers for limiting costs relies on forecasting medical costs and using it to manage premium and benefits programs. To get this information, in-house actuarial teams typically rely on medical claims to indicate utilization. This information is highly accurate because it is collected after the services have been rendered and includes actual costs.
However, this intelligence can come three months or more after the service is performed, leaving health plans a limited time to course correct. What if health plans were given utilization data before services have been rendered, to give earlier insight into utilization patterns and predict medical cost trends three months or more sooner than these methods? Health plans could potentially limit their higher-than-usual utilization and even work with providers to actively impact the total cost of care.
Early trend signal intelligence delivers projected medical trend three months earlier
Health plans using intelligent prior authorization for utilization management are digitizing and automating prior authorization approvals to save time for providers and drive earlier access to care for patients. But they can also use this data for another purpose: early indication of future utilization.
By applying machine learning models and using predictive analytics, intelligent prior authorization can predict future utilization trends using the following combination of data:
- Early trend signals: Based on prior authorization data, i.e., year-over-year (YoY) trend of authorization per 1,000 members (APK), forecasts the actual utilization trend up to three months in advance
- Previous projected APK: High and low range, incorporates YoY monthly trend, adjusted by business days, seasonality, and membership
- Projected utilization trend: Projects the high and low utilization trend for the year by leveraging early trend signals, layering on historic APK and claims seasonality, and adjusting by business days and membership
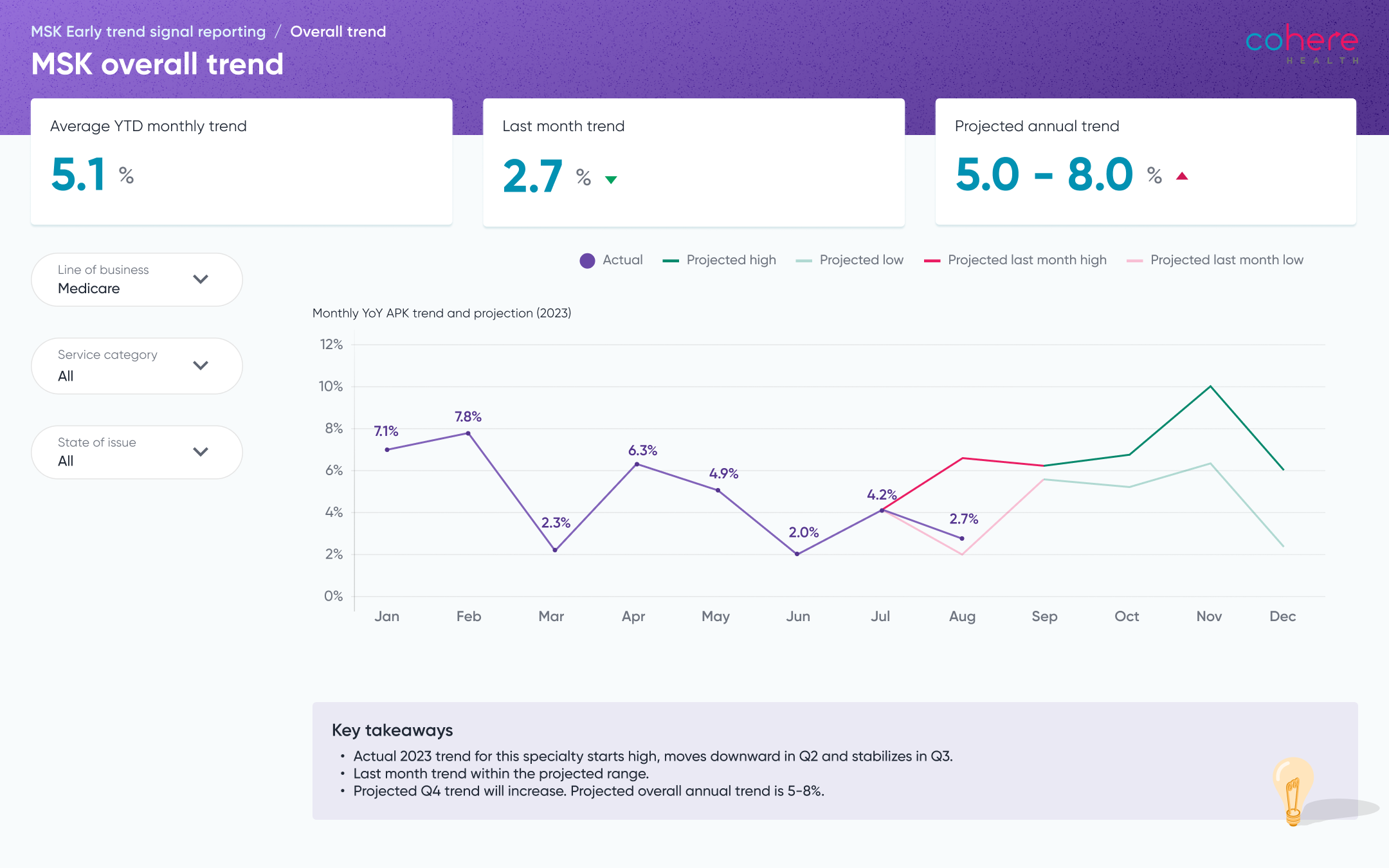
The health plan dashboard above shows an example of a health plan’s utilization trend. Based first on prior authorization data, it is augmented by historical data and then used to project future utilization for these services. As prior authorization data (and eventually, claims data) becomes available, the deviation can be measured, and health plans can promptly recalibrate their projections. This early trend signal intelligence can be used to:
- Identify high utilization to proactively manage medical loss ratio and inform benefit and premium design
- Augment utilization trend data with provider authorization data
- Collaborate with impacting providers on specific specialty or service category utilization
- Improve approval rate and experience with early feedback and actionable insights
Early implementation of this new technology has returned successful results. Cohere Health was able to accurately project higher quarterly medical trends using a combination of prior authorization and utilization data for high-volume services, the actual medical trend from previous quarters, and historic seasonality data.
Learn more about early trend signal intelligence in this white paper.