Federal and state government bodies are responding to physician and patient advocacy by driving new regulations intended to speed and standardize the prior authorization process. The regulations address issues that have been raised by the American Medical Association (AMA) and other industry groups concerning the undue burden of time-consuming, costly prior authorization processes that take away from a provider’s time with patients, and can delay appropriate care.
According to a 2020 AMA report, 90% of physicians state that prior authorization has had a negative impact on patients, and 30% report that prior authorization has “led to a serious adverse event for a patient in their care.” In a consensus statement from 2018, several national organizations, including the AMA, AHA, AHIP, and others, called for specific improvements to prior authorization. Two national sets of proposed rules introduced in recent months address these issues by requiring the following:
- Electronic prior authorization submission data exchange across payers, providers and patients, using application program interfaces (APIs) that are based on the HL7 FHIR standard
- Specific decision turnaround time standards, along with “real-time” prior authorization decision capability
- Transparency into prior authorization code lists, criteria, and reasons for denial
- “Goldcarding” capabilities to enable high-performing providers to skip the authorization process
In addition to the national proposals, there are many state-level proposals with similar and even additional requirements. While health plans would no doubt agree that improving prior authorization is important to better serve patients and providers, any one of the proposed requirements amounts to substantial effort and expense for a health plan to comply – in the aggregate, they will require heroic efforts. Instead of thinking about this as a compliance problem, forward thinking health plans are looking to transform their operations and technology. This opens up an opportunity to unite all constituents – the patient, provider and health plan.
What can forward-looking health plans do to ensure they are well-positioned for these regulatory changes?
1. Choose partners that provide broad prior authorization regulatory compliance capabilities.
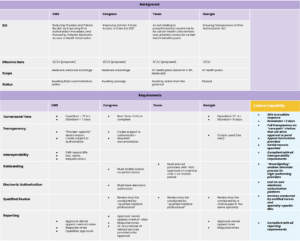
The new regulations in total represent a broad range of technological, timeliness, transparency, quality and reporting requirements. Some of these can be supported by innovative technology; others by high quality, efficient services with appropriate clinical oversight. Health plans are forced into a difficult choice: modernize legacy systems, or consider outside vendors for help. On the one hand, technology transformation projects are expensive, slow, and particularly difficult for smaller health plans. On the other hand, prior authorization tools and service vendors aren’t suited for a future focused on consumer quality, experience, affordability, and value. For example, outsourced benefit managers have substantial clinical management capabilities, but don’t integrate with provider systems; authorization portal vendors enable electronic submission, but don’t provide a complete, automated medical review to support rapid turnaround. Working with a prior authorization partner that supports compliance across the board will save time, money and effort, and increases the likelihood of timely, successful compliance. Below is a table summarizing some of the significant regulations on the horizon (there are many others at the state level), and how Cohere supports compliance:
2. Leverage compliance with prior authorization regulations as an opportunity to improve the patient/provider experience.
The broad regulatory compliance that the right partner can provide might elicit an audible “Phew!” and enable a better night’s sleep, but there’s even greater benefit in leveraging compliance to your strategic advantage. Automating authorization submission for the provider, as well as clinical reviews for your health plan, can connect your plan, your providers and your members on a single technology platform that enables the use of innovative technologies, such as machine learning, to further influence optimal care choices. For example, instead of using the required automation and interoperability to simply say “yes” or “no” to code-level service requests, your plan can use the same technology and content to inform patients and their providers about alternative, less expensive care options, more evidence-appropriate services, or higher quality downstream providers.
Cohere’s digital prior authorization solution not only supports regulatory compliance with end-to-end fully automated prior authorization, built on machine learning and other modern technologies; the solution also leverages that technology to (i) identify variations in care in real-time, and (ii) automatically recommend evidence-based alternative care options, called “nudges,” specific to the patient’s care episode or journey. The patient and all providers in the episode or journey are included, so that care is much better coordinated, while the system uses machine learning to continually refine guidance based on previous results. Our solution also enables “greenlighting,” or special paths for high-performing providers, as well as provider tiering, to recommend high-performing downstream providers. Our unique approach drives compelling results:
- 55% acceptance by providers of our alternative care “nudges,” in the authorization request workflow – when care decisions can still be affected
- 20% additional medical cost savings – above savings from a health plan’s current UM programs – from orienting to the episode of care, or journey, beyond a single specific service
For health plans or provider-led organizations such as ACOs, this provides much more than regulatory compliance – it provides the basis to activate patients and providers into technology-enabled care programs that will provide benefit far beyond processing an authorization request.