Cardiovascular
Using data and technology to enable care collaboration
Cohere’s fully-delegated delivery of our intelligent prior authorization solution for cardiovascular services helps health plans an end-to-end solution to drive better care outcomes, reduce provider burden, and save administrative costs.
- Encourages adherence to evidence-based care pathways
- Enables medex savings with upstream moments of influence
- Reduces care variation with increased decisioning transparency
- Applies patient and provider cohorting data to improve outcomes
The result?
Download our white paper to learn more about how we are aligning physicians and health plans to drive care collaboration and medical expense savings.
Powering our fully delegated solution for Cardiovascular services is Cohere Unify™, our intelligent prior authorization platform. Cohere’s platform brings together intelligent authorization intake, advanced technology, and real-time analytics with deep, evidence-based clinical intelligence, to enable the digital transformation of UM processes, driving greater operational efficiency, and most importantly, faster and better patient outcomes.
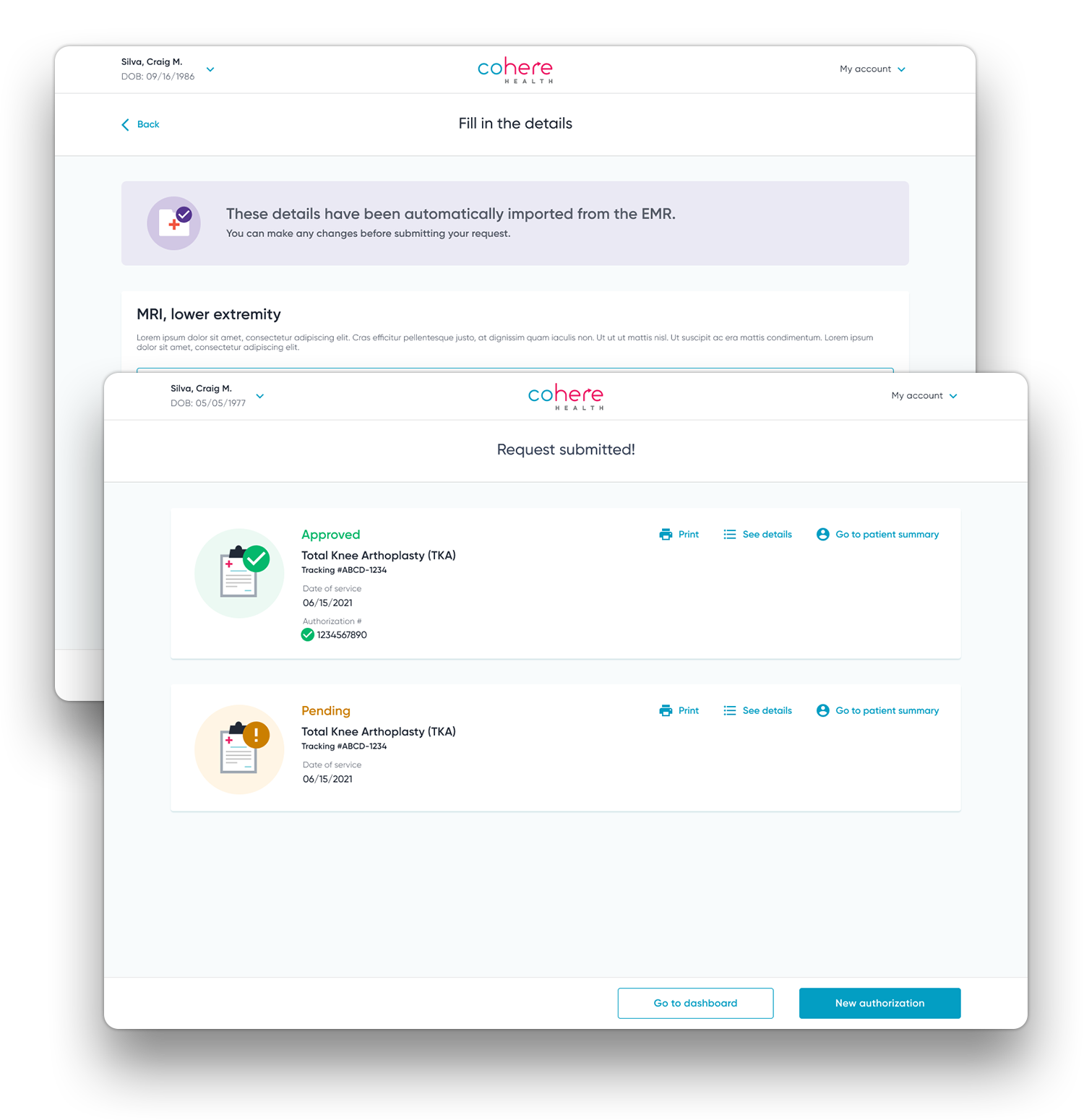
Foster collaboration with providers and patients by simplifying and improving the process
Our differentiated approach uses our board-certified cardiologists to drive impact
1
Drive optimal care using intelligent, diagnosis-centered care paths
Our platform creates patient cohort-specific care plans from 22 evidence-based, data-driven, cardiovascular care paths.
2
Influence care choices prior to request submission
Use in-workflow “nudges” during authorization requests to offer real-time guidance to patient-specific, clinically optimal care choices.
3
Reduce care variation by improving decisioning transparency
Leverage the longitudinal health record to provide pre-submission guidance and alignment to policy and best practices, improving utilization and patient outcomes.
4
Proactively leverage provider & patient data to improve outcomes
Different forms of health plan data can be used to approve higher quality care and inform health plans of strategic opportunities for cost savings and improved patient outcomes by suggesting underutilized services.
5
Interoperable, design-first, end-to-end automation
Our platform simplifies prior authorization for providers with digitized intake across multiple channels, automated decisioning for routine services and uses advanced technology to accelerate manual review, where required.