Reduce manual decision workload (dramatically)
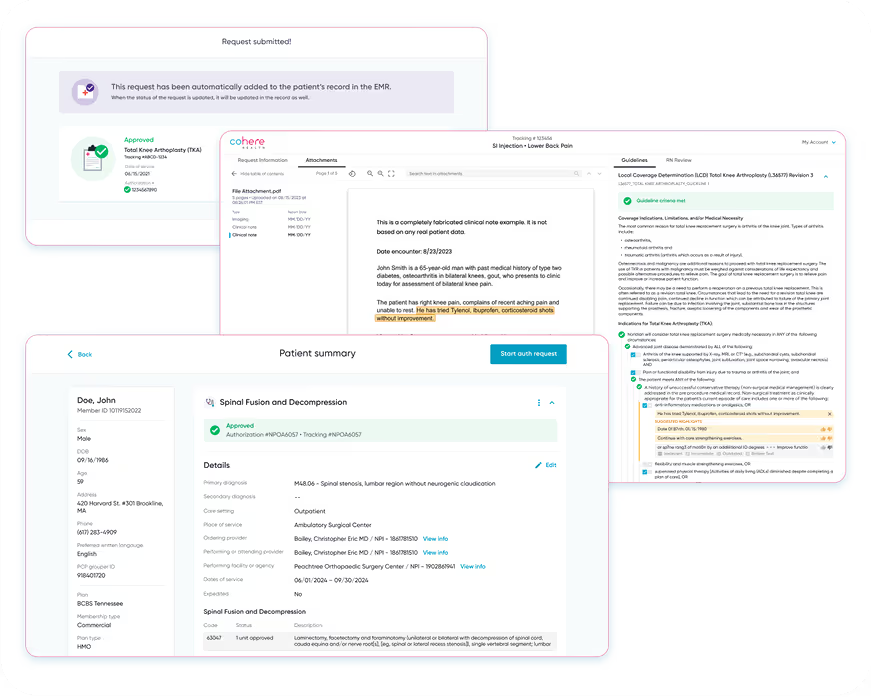
Our AI-powered automation handles the majority of prior authorization decisions, freeing your team to focus on complex cases that truly require human expertise. With approval rates of 50-90% depending on specialty, you'll see immediate impact on operational efficiency.