Managing the costs and complexities of cardiovascular care is a challenge for health plans. Often, health plans lack the necessary tools or data to coordinate a member’s care across multiple providers successfully. This gap makes it difficult to improve outcomes for chronic conditions. Our latest whitepaper explores how intelligent utilization management (UM) technology can help health plans and providers better collaborate to reduce waste, drive value, and improve outcomes.
Cardiovascular care is complex and often costly
Cardiovascular disease (CVD) has been the leading cause of death in the US for decades, resulting in over 700,000 deaths per year. Nearly half of all Americans are living with CVD. Consequently, the total direct and indirect healthcare costs for these patients are expected to reach $1.1 trillion by 2035.
Beyond its prevalence, cardiovascular care is also remarkably complex. It necessitates close coordination between numerous physicians and specialists, critical decision-making about testing and therapeutics, and the willingness of patients to adhere to long-term lifestyle changes. As a result, health plans often struggle to manage the costs, benefits, and overall value of their members’ CVD care.
Furthermore, there’s clear evidence of waste within the cardiovascular care landscape. A recent analysis found that, for one plan, unnecessary annual electrocardiograms (EKGs) and cardiac imaging accounted for 42% of their wasted dollars.
Cardiovascular care is plagued by variations in diagnoses and treatment, leading to additional costs and poorer outcomes.
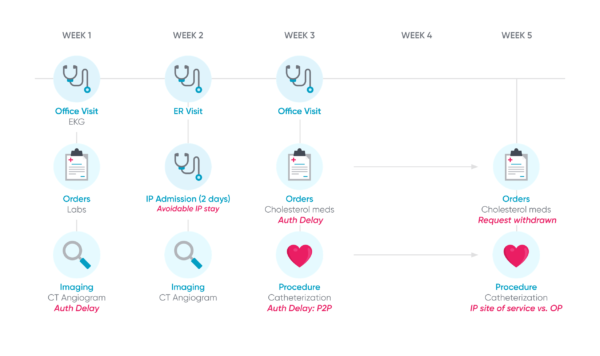
A typical cardiovascular care journey (below) helps demonstrate just how detrimental these compounding factors can be for just one patient. Hazel’s care was unnecessarily delayed and costly from avoidable ER and hospital visits to prior authorization delays. As a result of this convoluted timeline, both she and her cardiologist are left feeling frustrated.
Typical Patient Journey for Chest Pain/Coronary Artery Disease
Leveraging intelligent technology to simplify and improve cardiac care
Supporting the patient’s whole care journey across multiple physicians, sites of service, and episodes are critical to improve outcomes, especially for chronic conditions. The emergence of collaborative, AI-driven utilization management technology allows health plans to finally address the fragmentation of care decisioning and care delivery. Below are just some of the ways the Cohere platform can drive value in cardiac care and improve both patient and provider experiences:
- Partnerships to improve care: In 2021, Cohere partnered with the American College of Cardiology (ACC) to drive improvements in care quality and generate medical cost savings by increasing the use of gold-standard medical guidelines. By partnering with Cohere, the ACC seeks to ensure more complete utilization of its evidence-based guidelines by primary care physicians (PCPs) and cardiologists across the country.
- Quicker time to accurate diagnoses: Patients are placed on cardiology care paths that enable Cohere’s intelligent UM platform to offer automated, evidence-based guidance at the point of authorization, helping providers make the most valuable decisions. By ensuring that the vast majority of prior authorizations are approved within one day, the platform allows providers and patients to avoid the complications and frustrations of delayed care.
- Better procedure selection leads to better outcomes: When a patient requires an invasive evaluation or an interventional procedure, Cohere’s platform helps avoid unnecessarily aggressive treatment by requesting proper documentation of the indication(s). The platform can also:
- Analyze the patient’s calculated risk score, accounting for their previous healthcare utilization, and deliver in-platform recommendations for a procedure that meets ACC guidelines or appropriate use criteria
- Indicate when a patient is a good candidate for moving directly to surgical intervention
- Help PCPs and cardiologists identify top-performing specialists for a referral at the point of authorization
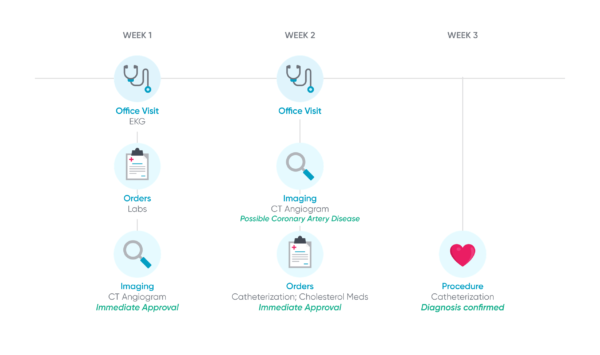
The Cohere journey (below) illustrates a stark contrast compared to the typical cardiac patient journey above. The visuals demonstrate how important an intelligent UM platform can be for:
- Supporting providers’ ability to care for their patients
- Decreasing unnecessary steps and delays
- Improving the overall value and experience for each patient’s care journey
The Cohere Patient Journey for Chest Pain/Coronary Artery Disease
Download the full whitepaper here to learn more about how health plans can benefit from an intelligent UM platform to deliver high-value, cost-effective cardiac care at scale.
________________________________________________________________________________________________
About the Authors:
Susan Bennett, M.D., Associate Medical Director of Cardiology
Dr. Bennett is a non-invasive consulting cardiologist practicing in both metropolitan and rural areas for over 25 years, specializing in echocardiography and preventive cardiology. She serves as an Associate Medical Director of Cardiology at Cohere Health. Dr. Bennett created and established the George Washington University Women’s Heart Program, one of the first in the country. She trained in Internal Medicine at Barnes Hospital, Washington University of St. Louis, then in Cardiology at the Hospital of the University of Pennsylvania and University of Maryland in Baltimore.
Marie Parker, Cardiology Clinical Program Leader
Marie Parker leads Cohere’s Cardiology Clinical Program, bringing over 15 years of experience in developing, implementing, and evaluating chronic disease programs to improve quality across various sectors of the healthcare ecosystem. In addition to board certification in pharmacotherapy and healthcare quality, she holds a doctor of pharmacy degree from the University of Georgia and both a master’s degree (Emory University) and a doctor of philosophy degree (Georgia State University) in public health.

