For patients with diabetes, coronary artery disease is the most important cause of mortality. Intelligent prior authorization uses advanced technology to reduce care variation, promote high-value care, and improve outcomes for cardiology patients.
Diabetic patients have increased risk of coronary artery disease
Having diabetes increases a patient’s risk of coronary artery disease (CAD) by two to four times. CAD is the most important cause of mortality in these patients with diabetes.
After the COVID-19 pandemic, the national heart disease death rate reversed its previous decline, creating a 4% increase from 2019, closer to the 2015 rate, representing approximately five years of lost progress among all adults. CAD accounted for 55% of total heart disease deaths in 2020.
Fortunately, health plans can leverage cutting-edge innovations in prior authorization technology to improve outcomes and save medical expenses.
How health plans can use intelligent prior authorization to help improve care for cardiology patients
Intelligent prior authorization orients prior authorization transactions within the broader context of the patient care journey to help improve outcomes. By leveraging patient data before the transaction is approved, intelligent prior authorization can help reduce care variation and align health plans and providers on evidence-based, high-value care for complex patient populations.
Encouraging evidence-based medicine: Risk-stratifying CAD
One condition that intelligent prior authorization has been focusing on is coronary artery disease (CAD), the leading cause of death in the United States. With the United States spending $320 billion annually in 2016 managing and treating CAD and cardiovascular risk factors (cardiovascular spending), Cohere is targeting this population to encourage high-value care pathways and reduce total spending.
According to evidence-based research conducted by cardiology societies such as the American Association of Cardiology, myocardial perfusion imaging (MPI-SPECT) is most useful in symptomatic patients with an intermediate likelihood of angiographically significant CAD. Cohere identified this expensive and sometimes unnecessary test as a perfect opportunity to leverage technology to align providers on appropriate high-value care. Using the pre-test probability risk chart below, Cohere deploys behavioral change notifications at the point of the service request, such as “nudging” providers to consider an alternative, lower-cost, less invasive test where appropriate, such as a coronary artery calcium score, routine exercise treadmill, CCTA or a stress echo.
Table 5 Pre-test probabilities of obstructive coronary artery disease in 15 815 symptomatic patients according to age, sex, and the nature of symptoms in a pooled analysis of contemporary data
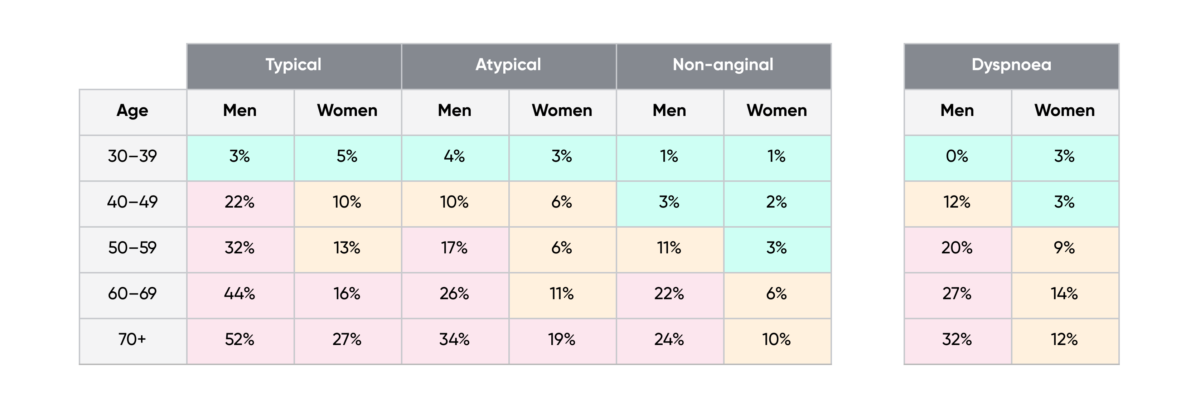
CAD = coronary artery disease; PTP = pre-test probability
In addition to the classic Diamond and Forrester classes, patients with dyspnoea only or dyspnoea as the primary symptom are included. The regions shaded light pink denote the groups in which non-invasive testing is most beneficial (PTP >15%). The regions shaded beige denote the groups with PTPs of CAD between 5-15%, in which testing for diagnosis may be considered after assessing the overall clinical likelihood based on the modifiers of PTPs presented in Figure 3.
With only the intermediate or high-risk patients requiring advanced imaging such as an MPI-SPECT test, health plans can reduce the total cost of care for this population and collaborate with physicians to encourage evidence-based medicine, reducing variation.
There is a caveat for diagnosing CAD for patients with diabetes. Most importantly, the greater incidence of silent ischemia in diabetic patients means they are less likely to experience exertional angina or chest pain with exercise testing, making diagnosis more difficult.
Nevertheless, several studies have demonstrated that using stress MPI produces comparable diagnostic results in patients with and without diabetes. Appropriate use criteria from cardiology societies suggest patients with a high ten-year atherosclerotic cardiovascular disease risk (ASCVD) risk of greater than or equal to 20% for which diabetes is a significant risk factor, a stress MPI-SPECT even in asymptomatic patients, may be appropriate.
Mining clinical data to treat patients upstream: Care management programs
For cardiology patients, many “whole patient” factors can increase the risk of CAD or other serious conditions, including smoking, poor diet, and lack of exercise. If physicians could encourage improvement in these areas, the patient’s cardiovascular health would also likely improve.
Consider the evidence below:
- Quitting smoking after a heart attack or cardiac surgery reduces the risk of all‐cause mortality among patients with CAD by 36%.
- Despite the inverse association between Ultra Processed Foods (UPF) consumption and cardiovascular health score, 67% of American adolescents consume UPF daily.
- Exercise training can improve insulin sensitivity, lipid profile, vascular reactivity, and cardiorespiratory fitness, particularly in type 2 diabetes mellitus patients with cardiovascular comorbidities.
Cohere uses artificial intelligence (AI) and machine learning to encourage the treatment of the whole patient and improve patient outcomes.
When a provider includes patient information in their authorizations for a cardiac intervention, our intake solution uses optical character recognition (OCR) and machine learning to scan the clinical attachments and match the patient to a cache of data for patients with similar clinical backgrounds, called a patient cohort. Evidence-based guidelines identify opportunities to improve care for the patient, such as enrollment in a health plan’s care management program.
At the point of the prior authorization request, an in-platform nudge suggests enrollment in a smoking cessation or nutrition program.

Episodic authorizations can make the process even more streamlined by bundling the authorization for cardiac rehabilitation with coronary intervention. Episodic authorizations encourage patients and providers to use clinical pathways that promote the best intervention outcomes, reducing the risk of further complications and added expense.
As part of a medical school project to alter my cardiovascular risk factor profile, I started participating in endurance running. An interest in athletics and cardiovascular physiology is one of the reasons I became a cardiologist. I continue to participate in endurance sports such as cycling.
To learn more about how our end-to-end outsourced utilization management solution, Cohere Complete™, improves outcomes and reduces costs for cardiology patients, download our white paper.
