/
Blog/
Breaking down silos: Why future cost containment demands a connected approach across UM, Claims, and PIBreaking down silos: Why future cost containment demands a connected approach across UM, Claims, and PI
Published:
September 3, 2025

Health plans have chased cost containment at every stage of the claim lifecycle, but returns are shrinking, provider abrasion is rising, and administrative costs are at all-time highs. What if the solution is not doing more of the same thing, but thinking fundamentally about new ways to approach the problem?
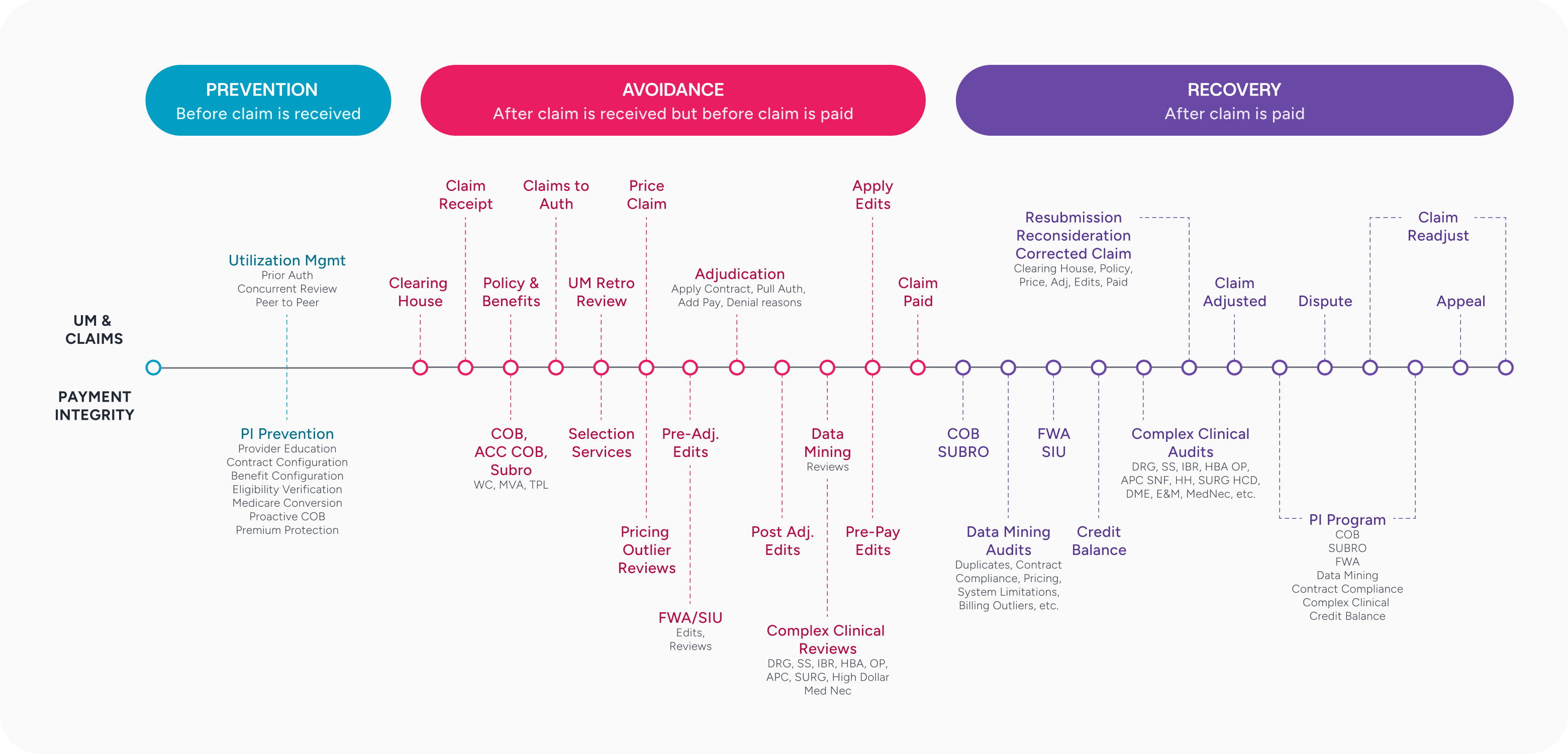
In this blog, we demonstrate how a unified approach where Utilization Management (UM), Claims, and Payment Integrity (PI) capabilities intersect provides more opportunity than standard PI programs alone.
The hidden cost of fragmented thinking and operations
For decades, health plan cost containment strategies have operated in silos. UM teams focus on containing costs based on prior authorization processes, claims do so on auto-adjudication, and PI teams prioritize complex clinical and coding reviews. For years, there has been a trend in PI to shift left. UM, specifically prior authorization (PA), is a cost containment strategy that is as far left as you can get in the life cycle of a claim. The PA process ensures that services are medically necessary and appropriate for the patient. Providers share clinical documentation with a health plan for the initial PA, ongoing status (concurrent), and a discharge summary for inpatient stays. The data collected for UM decisions, and many of the UM processes, overlap with data and processes in PI reviews (pre-pay) and audits (post-pay). However, there is very little cross-pollination between functions.
Each function is optimized in isolation, with unique processes, teams, and potential provider touchpoints. The result? Duplicated efforts, inefficiency, and growing frustration for health plans and providers.
Additionally, providers navigate multiple, disconnected approval processes throughout this lifecycle. Different health plan teams also request and review clinical documentation multiple times. While these silos can be viewed as standard operational complexities, critical cost containment, quality, efficiency, and provider satisfaction opportunities are overlooked between functions. The processes and data already exist—what’s missing is connection.
The convergence opportunity
Innovation and untapped value often arise when different processes, people, and technologies intersect. In this case, at the intersection of three specific capabilities, UM, Claims, and PI, lies an untapped opportunity for cost containment potential that dwarfs what any single function can achieve alone. When these inputs are combined, health plans can make faster, more accurate decisions. The real opportunity lies not in incremental efficiency but in a shift toward proactive, connected cost containment.
We see this most clearly in three areas:
1. Claims to auth matching
Matching a claim to an authorization is neither simple nor straightforward. Health plans attach an authorization to a claim based on claims-to-authorization matching rules to ensure accurate claim payment. These basic rules often miss important clinical context and create payment errors. Data, clinical, and claim expertise are needed to ensure the specific criteria and applicable exceptions are considered. The quality of the “claims to auth match” process is directly correlated with the accuracy of the adjudication of a claim. A new precision approach is needed to improve quality and increase the percentage of accurate attachments. Minimizing incorrect attachments and incorrect “no auth” determinations will reduce the risk of payment errors.
The intersection of UM, Claims, and PI capabilities provides a new opportunity to avoid payment errors and reduce rework. By expanding basic claims to precision auth matching functionality that includes the full clinical picture, more data, and considers more complex encounters, authorizations can be more accurately matched across facility and professional charges.
2. PI selection
Over the past two years, significant progress has been made to enhance audit capabilities, particularly for inpatient claims. Current DRG metrics demonstrate excellent quality and efficiency gains by using natural language processing models (NLP) and other AI systems when performing reviews and audits.
As an industry, we have also improved performance by refining our selection queries to improve hit rates and savings amounts. A new trend is to use alternate and enriched data in addition to claim data to reduce the risk of false positives. Pricing data and provider profiles are examples of alternate data sources currently used by some PI teams.
In 2024-2025, we saw a shift toward enhancing payer-provider collaboration. A combination of UM, Claims, and PI data and expertise will further this collaboration and improve the quality and speed of evaluating a claim’s risk for payment error. If a review of the clinical documentation submitted by the provider supports the DRG coding, diagnosis, and procedure codes, the claim can be flagged as clinically validated. This means it can be assessed as having a lower risk of overpayment shortly after the claim is received.
3. PI Medical necessity reviews
Despite progress in previous categories, this area is subject to significant inefficiency. UM teams with deep clinical and regulatory expertise complete medical necessity reviews, which are often listed as a specific Payment Integrity exclusion. The rationale is that if services have a prior auth approval, a claim should not be re-reviewed for medical necessity.
Health plans are under extreme pressure to reduce administrative costs while maintaining payment integrity. There is a subset of claims that offer an opportunity to leverage intersecting capabilities between UM and PI that can help meet this challenge.
To highlight this opportunity, let’s consider an inpatient claim received without authorization. This could include a claim for a non-par provider, a provider with an auth exception, or an ER admit with no notification or request for approval. It is not uncommon for both UM and PI teams to complete separate medical necessity (UM) and complex clinical and/or coding validation (PI) reviews on the same claim. The reviews are not redundant as they have separate goals, but there is a duplicative effort in reviewing the clinical documentation.
Same provider(s). Same clinical documentation. Separate processes. Separate timelines. Separate provider touchpoints.
Combining medical necessity and complex clinical and coding reviews, backed by clinical, regulatory, and operational expertise, improves quality, efficiency, and turnaround time.
The big picture of connected efficiency to shift left
This isn’t just about creating efficiency and cost-containment opportunities. This fundamental reimagining of cost containment shifts from a reactive and siloed process to a proactive and optimized approach focusing on prevention and cost avoidance. Breaking down silos across UM, Claims, and PI is how health plans can move closer to real-time payments and set a new industry standard. The future is available today for forward-thinking organizations. Learn more about how our AI-powered payment integrity solutions can modernize your PI strategy at coherehealth.com/payment-integrity.
Available For Download
Written by

Monique
Pierce
Monique has 25+ years experience building and leading payment integrity teams. She has worked for both small start-up regional health plans like Oxford Health and Devoted Health as well as large national health plans like UnitedHealthcare. Monique also has extensive leadership experience in the vendor partner space including Optum, SCIO Health Analytics and EXL. Monique is known for her vision and ability to execute as well as her passion for metrics. Today, Monique is driving opportunities to improve claim payment by designing and developing a bridge between prior auth and claim reconciliation products at Cohere Health.
Stay ahead with expert insights on transforming utilization management and payment integrity—delivered straight to your inbox.