The passage of CMS-0057-F includes key prior authorization provisions to improve interoperability, turnaround times, transparency, and accountability. Of the frequently asked questions about the final rule we’ve received, intelligent prior authorization rises to the surface as the strategic choice for health plans seeking to satisfy the requirements.
Answering frequently asked questions about the changes coming to prior authorization
How will implementing standard APIs help health plans make the transition to greater interoperability?
The prior authorization process is fraught with delays and manual oversight. One of the contributing factors to this problem is the volume of information that is exchanged during the process. To help improve the speed of this data exchange, CMS has identified five APIs that health plans will need to systematize:
- Patient Access API
- Provider Access API
- Provider Directory API
- Payer-to-Payer API
- Prior Authorization API
Health plans serving Medicare and Medicaid patients that implement the infrastructure and technology to support this transition proactively will find themselves well-situated to navigate compliance with the rule and future regulatory changes to the prior authorization landscape.
As an initial step to implementing electronic prior authorization, disparate data must first be sorted and converted to a single format. The new rule will standardize information by requiring health plans to implement the five APIs above. Here are the formats that they are requiring for each:

With this regulation, plans will be taking the first step to reducing the administrative burden of prior authorization. Clean and standardized data is prepared for incorporation into more automated processes.
What strategies can health plans explore to improve their turnaround times before the rule takes effect in 2026?
The new CMS final rule will require health plans to comply with tightened turnaround times by January 1, 2026. Health plans will need to deliver decisions for standard requests within seven days and expedited requests within 72 hours. With this new regulation, CMS is working to hasten patients’ access to appropriate care, which in turn will improve outcomes. Eighty-nine percent of physicians cite prior authorization as negatively impacting their patients’ clinical outcomes.
Cohere supports tightened turnaround times and recommends that health plans implement intelligent prior authorization solutions to ensure regulatory compliance. By digitizing prior authorization submissions and using machine learning and large language models to analyze patient information, intelligent prior authorization can automatically approve the majority of cases. The effect of this instant decision is staggering. By delivering instant decisions to physicians, patients can receive approval at the point of care, allowing them to schedule subsequent services sooner.
Intelligent prior authorization also accelerates the turnaround time for more complex cases that still require manual clinical review. Machine learning models extract the most relevant sections of patient information, prepopulating reviewer checklists, and highlighting documents as supporting evidence for clinical reviewers, saving them precious time as they review expedited and standard prior authorization requests.
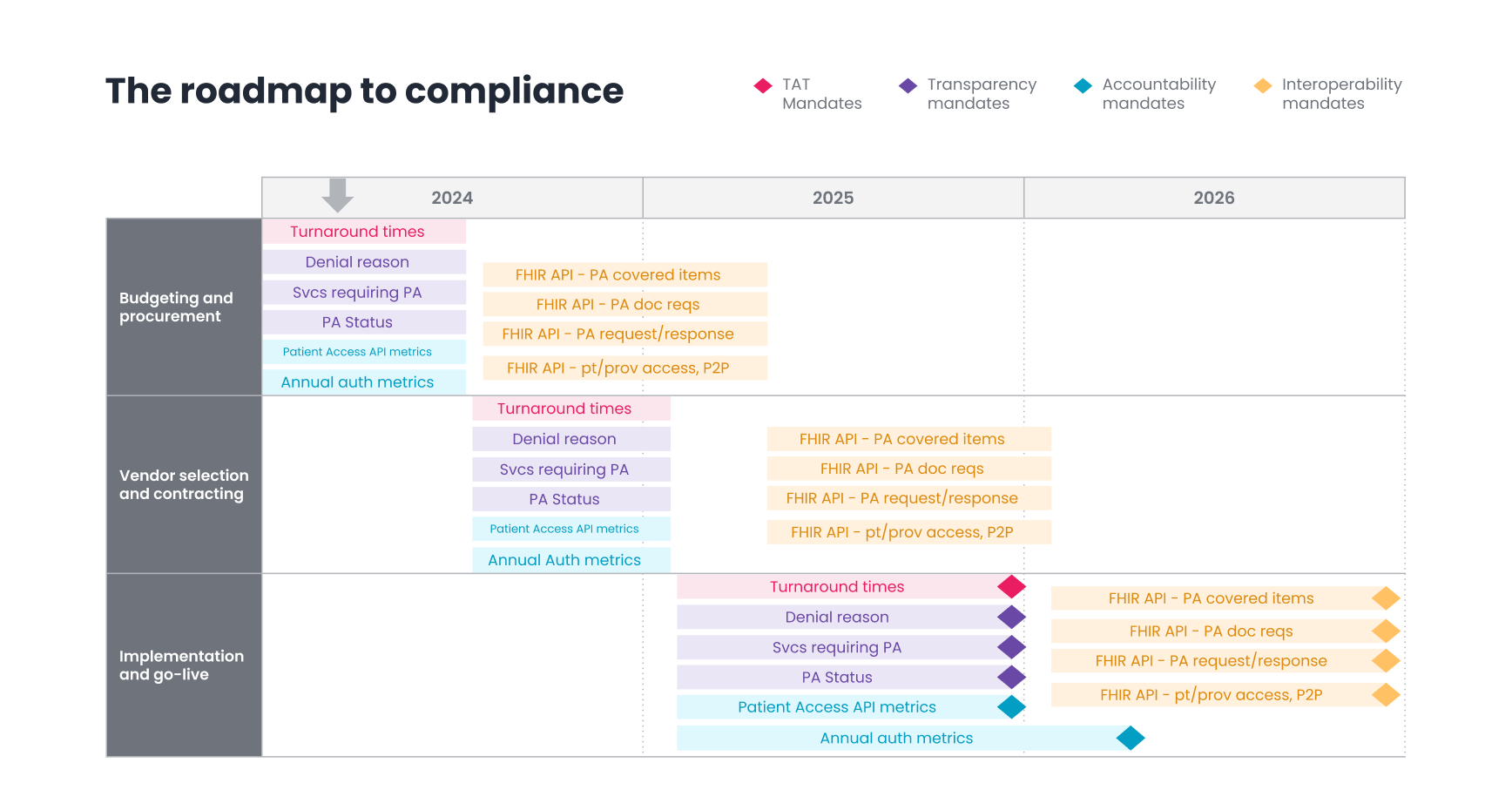
While the deadline for this implementation might seem far away, health plans should already be started on their compliance strategy. Plans should have their budgeting and procurement planning approval completed by the middle of 2024. It will take the next six to nine months for procurement, vendor selection, and negotiation, which will bring plans into early 2025. Implementation within the existing technological infrastructure will also take another six to nine months, bringing plans to the end of 2025. This timeline will enable plans to go live at the end of 2025 and smooth out the process just in time for the 2026 deadline. There’s no time to waste!
What role can technology play in greater transparency for physicians?
For physicians, the current prior authorization system is like trying to play a game without knowing the rules. Currently, there is no requirement for transparency, so physicians may not know what evidence is required to get approval for a prescription or procedure. When the physicians don’t know the rules, patients lose.
The new guidelines outlined in the final CMS rule will require health plans to communicate their requirements and denial reasons to physicians. Physicians can ensure that all criteria are met before submitting an authorization, instead of learning which information is missing after the request has been sent. This will reduce wasted time on administrative back and forth, with either a reviewer, in a peer-to-peer, or through an appeals process.
Using intelligent prior authorization makes it easy for physicians to see the requirements when they are sending the request. In-app notifications alert them of missing information before the request is submitted. Additionally, health plans and physicians can work collaboratively to improve the rate of auto-approvals. For example, a health plan may request a physician reduce the number of visits in a request for physical therapy to meet the requirements, so instead of pending for manual review (and delay), an auto-approval would allow the patient to schedule care immediately.
With the new rule’s requirements, physicians must be notified of the health plan’s decision. Intelligent prior authorization enables practices to easily check the status of their requests using the same platform where they requested them. Physicians must already use so many different platforms. Cutting down on the places where they have to go will save them time and go a long way in improving the relationship between health plans and physicians.
How will publishing prior authorization metrics help improve accountability?
While prior authorization is a necessary process to ensure that patients are receiving appropriate care and to reduce healthcare costs, many patients and physicians complain that they cannot see behind the curtain. Improving transparency between those involved will level the playing field between stakeholders. The CMS final rule requires health plans to publicly publish their prior authorization metrics on their website or via publicly accessible hyperlinks annually.
Cohere actively facilitates this type of transparency between physicians and health plans. Today, we deliver scorecards on a quarterly basis to our health plan partners. This is an important step to ensuring physicians and health plans have insight into their performance and how they can continually improve and deliver better care. This transparency also encourages health plans to become more accountable and can improve tension between physicians and health plans.
The future of prior authorization
As health plans work to implement new systems to achieve regulatory compliance with CMS-0057-F, the prior authorization process will see improvements in interoperability, turnaround times, transparency, and accountability.
Watch our webinar with AHIP to learn more about the final rule’s prior authorization provisions and how Cohere’s intelligent prior authorization can help health plans with their compliance strategy.