How health plans can prepare
On January 17, 2024, The Centers for Medicare & Medicaid Services (CMS) finalized a rule to advance interoperability and improve prior authorization for Medicare and Medicaid patients. At Cohere Health, we are especially encouraged by the stipulations for improving prior authorization included in the rule and see it as a step in the right direction. This initiative will improve transparency, reduce physician burden, and lead to faster patient access to care. Cohere sees the CMS final rule as an opportunity for plans to evolve from transaction-focused prior authorization to transformational utilization management—an approach that improves the whole patient journey and enables more successful value-based care arrangements. The implementation of intelligent prior authorization is the first step in this evolution.
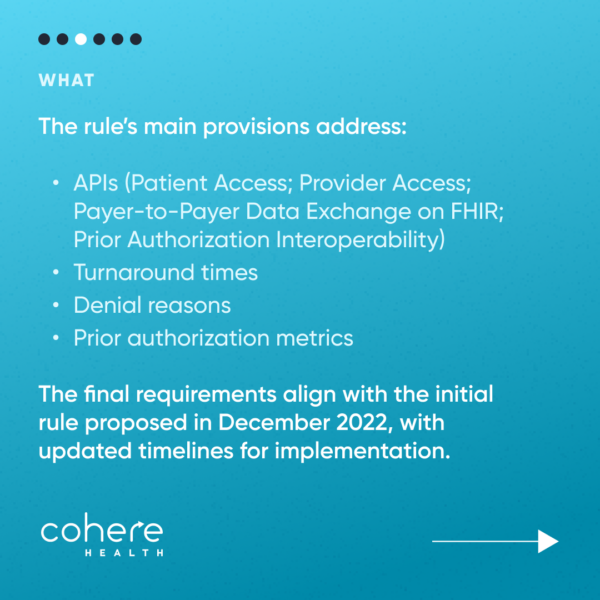
The final rule is based on the Advancing Interoperability and Improving Prior Authorization Proposed Rule, published in December 2022. Cohere provided feedback to CMS during the rule’s comment period last spring. The final rule remains largely similar to its proposal. However, some key differences include:
- The implementation deadline for FHIR-based APIs was pushed back to January 1, 2027. However, payers must publish metrics on Provider API usage by January 1, 2026
- CMS announced an enforcement discretion of HIPAA X12 278 standard for interoperability APIs
- Health plans are required to publish their first metrics around authorization rates by March 1, 2026.
- Authorization status was added to patient access, provider, and payer-to-payer APIs
- Qualifying health plans on federally facilitated exchanges are excluded from the turnaround time requirements of 72 hours for expedited requests and seven days for standard requests
Health plans serving Medicare and Medicaid patients that implement the infrastructure and technology to support this transition proactively will find themselves well-situated to navigate compliance with the rule and future regulatory changes to the prior authorization landscape.
Here are four changes to prior authorization in the new CMS final rule
- Health plans will be required to build and maintain a Fast Healthcare Interoperability Resources (FHIR) Application Programming Interface (API) that has a list of covered items and services, can identify documentation requirements for prior authorization approval, and supports a prior authorization request and response by January 1, 2027.
These prior authorization APIs must also communicate whether the payer approves the prior authorization request (and the date or circumstance under which the authorization ends), denies the prior authorization request (and a specific reason for the denial), or requests more information.
This requirement would ease the provider burden by establishing clear, instantaneous communication on whether a prior authorization is required, which patient information and documentation is needed to evaluate appropriateness, and accelerating and automating additional information requests and final prior authorization decisions, for a selected service.
Cohere’s intelligent prior authorization solution, Cohere Unify™, helps providers determine if a prior authorization is required and digitizes prior authorization intake across all channels, including fax, portals, and EMRs. The solution includes in-platform nudges that automatically prompt for missing information before the request is submitted, and uses artificial intelligence to incorporate relevant patient information from the EMR. The solution also provides intelligent decisioning, based on clinical evidence, NCD/LCD, and plan-specific policy guidelines.
Cohere already has FHIR-based APIs in production today (PAS, CRD, DTR).
- Health plans will be required to communicate the reason for denial with the physician, regardless of the channel used to submit the request by January 1, 2026.
By requiring plans to communicate with physicians and their staff after issuing a denial, health plans will provide context for their evaluation process and increase transparency between themselves and providers. This additional insight into the decisioning guidelines will help providers who repeatedly submit requests for the same procedures and may result in the submission of corrected requests in cases rejected due to missing or incomplete information.
Cohere’s intelligent prior authorization solutions were developed around the fundamental principle of increasing transparency between providers and health plans to deliver faster approval of quality care for patients. By improving interoperability, and the secure exchange and utilization of health data, payers and providers can work together to deliver better outcomes for patients. Cohere’s platform provides reasoning for denials, and the care path guidelines used to intelligently decision authorization requests are publicly available.
- CMS will now require a shorter turnaround time for urgent and nonurgent requests, with a timeframe of 72 hours for urgent and seven days for non-urgent requests. This provision goes into effect January 1, 2026.
The rule will require impacted payers (excluding qualifying health plans on the federally-facilitated exchanges) to send prior authorization decisions within 72 hours for urgent requests and seven days for standard requests. Currently, the long wait times between request submission and authorization decisions delay patients’ access to care. These delays present additional problems for patient populations affected by social determinants of health, where service delays can affect the continuity of and access to care.
With the digitization of prior authorization offered by Cohere’s intelligent prior authorization solutions, 83% of requests are immediately approved. This leads to faster access to care and ultimately delivers better outcomes. In the small number of cases where clinician review is required, Cohere averages a 4.5-day turnaround time and only nine hours for expedited cases.
- Health plans will be required to publicly publish certain prior authorization metrics annually, with the first set of metrics to be published by March 1, 2026.
CMS will require impacted payers to publish the following metrics: a list of all items and services that require prior authorization; the percentage of prior authorization requests that were approved, denied, approved after appeal, and approved after an extension was granted, for each standard and expedited requests; and median turnaround times, for each standard and expedited requests.
To increase transparency around authorization decisions, health plans would be required to publish prior authorization metrics on their website. Cohere supports this proposed requirement and the usage of prior authorization metrics to improve the overall quality of care for patients. When all of the stakeholders in the utilization management process have transparency around metrics, it is possible to move toward value-based care. At Cohere, we have our own policy of sharing metrics quarterly with health plans.
Cohere is encouraged by the progress made with the finalization of the CMS final rule and its focus on improving the cumbersome prior authorization process.
You can read the full requirements of the Interoperability and Prior Authorization Final Rule, here.
Download our white paper, How keeping up with CMS regulatory changes will drive better patient outcomes, to dive into how intelligent prior authorization can help plans comply with federal regulations while improving utilization and patient outcomes.