Episodic authorizations are a uniquely valuable feature of intelligent prior authorization, which enables upfront, combined authorization of multiple services expected for a specific patient episode. An ideal episodic authorization is driven by a combination of patient cohort data, predictive analytics, and evidence-based medical research. Health plans can use episodic authorizations to encourage high-value care across the patient journey, significantly reduce provider and plan burden, and help patients receive care faster!
1. What are episodic authorizations?
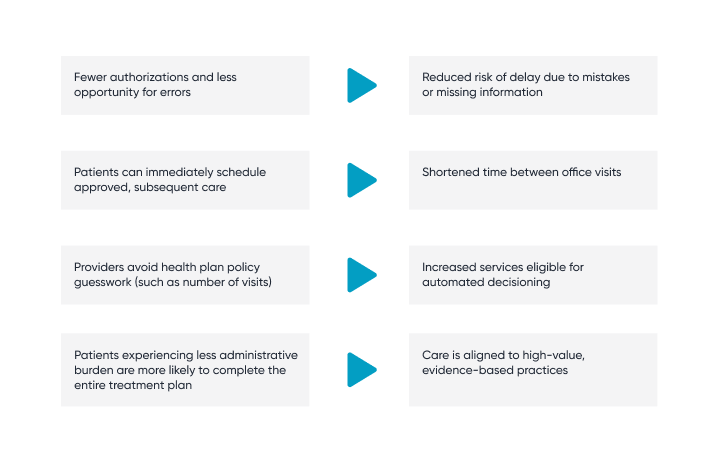
Episodic authorizations anticipate and consolidate multiple authorization requests for a care episode. They are triggered by a high-profile medical event and occur during a discrete care episode. By requiring only one prior authorization for multiple services, spanning different providers and locations, health plans reduce administrative burden, encourage treatment alignment to best practices, and shorten the care episode for the patient.
2. How do episodic authorizations advance health equity?
A KFF survey found that 16% of all insured adults experienced prior authorization problems in the past year. Certain risk factors, such as an economic situation or access to physician networks, known as social drivers of health (SDOH) increase patients’ likelihood of experiencing issues:
- One in four adults enrolled in Medicaid experience prior authorization problems—double the risk of a Medicare enrollee experiencing issues.
- Patients using more healthcare services increase their likelihood of experiencing problems:
- Patients with more than 10 visits had three times the risk of patients with two or fewer visits.
- Seeking treatment for mental health conditions doubled the chance of adults experiencing prior authorization problems (in general).
- Patients with diabetes have a 64% higher risk of experiencing prior authorization issues than those without.
- Despite federal regulation prohibiting private plans from requiring prior authorization for medical services in an emergency room, there was a correlation between patients who had received care in the emergency department (ED) within the last year and those experiencing prior authorization issues. Patients in the ED were twice as likely to have reported issues.
Leveraging health plan data, intelligent prior authorization can use episodic authorizations to automatically suggest in-network providers, specific to the patient’s condition and location, thus being more likely to drive better and faster health outcomes.
Episodic authorizations reduce administrative burden. By grouping a series of services and approving entire care episodes with a single transaction, intelligent prior authorization can improve the process for patients.
3. How do episodic authorizations work with care paths to reduce care variation and improve quality?
Episodic authorizations can encourage appropriate, high-value care further upstream by using prior authorization transactions as “moments of influence.”
For example, when a provider submits a request for a high-profile event (like surgery), intelligent prior authorization solutions can suggest, with episodic authorization, a bundle of recommended subsequent services to accelerate full recovery. Automatically approving these services can allow offices to immediately schedule the patient for subsequent care and increase the likelihood of the patient completing the entire care path.
Experiencing prior authorization problems made a person three times more likely to report being unable to receive medical care or treatment recommended by a medical provider (34% vs 10%) and about three times more likely to report significant delays in receiving medical care or treatment (32% vs 11%) than those who did not. People who experienced prior authorization problems were about twice as likely to say their health declined as a direct result (26% v 11%).
So, with episodic authorizations, both the patient and the provider benefit. The providers get the added benefit of reduced administrative burden and avoid the guesswork of health plan policy specifics like number of visits or site-of-service, while patients get on a faster path to recovery.
4. How is Cohere Health leveraging episodic authorizations for better MSK outcomes?
Total knee arthroplasty (TKA) is a good example of how Cohere uses episodic authorization to improve outcomes. When a provider submits a TKA authorization request, if Cohere’s decisioning engine automatically approves the request, it also proactively initiates and approves requests for post-operative physical therapy and then alerts the provider and the patient of all services that have been approved. As a result, providers experience decreased administrative burden because there is no need to submit a duplicate authorization request for post-operative therapy.
Favorable signals indicate that episodic authorizations encourage more timely physical therapy usage. The earlier patients start post-operative physical therapy, the more favorable their recovery: patients who start therapy on the first postoperative day require less pain medication and reduce their risk of 30-day readmission.
To see the results from Cohere’s episodic authorizations pilot, download our white paper, How episodic prior authorizations are powering MSK care management transformation.