Cohere Complete™ Outsourced Utilization Management
Partner with Cohere to transform specialty benefit management
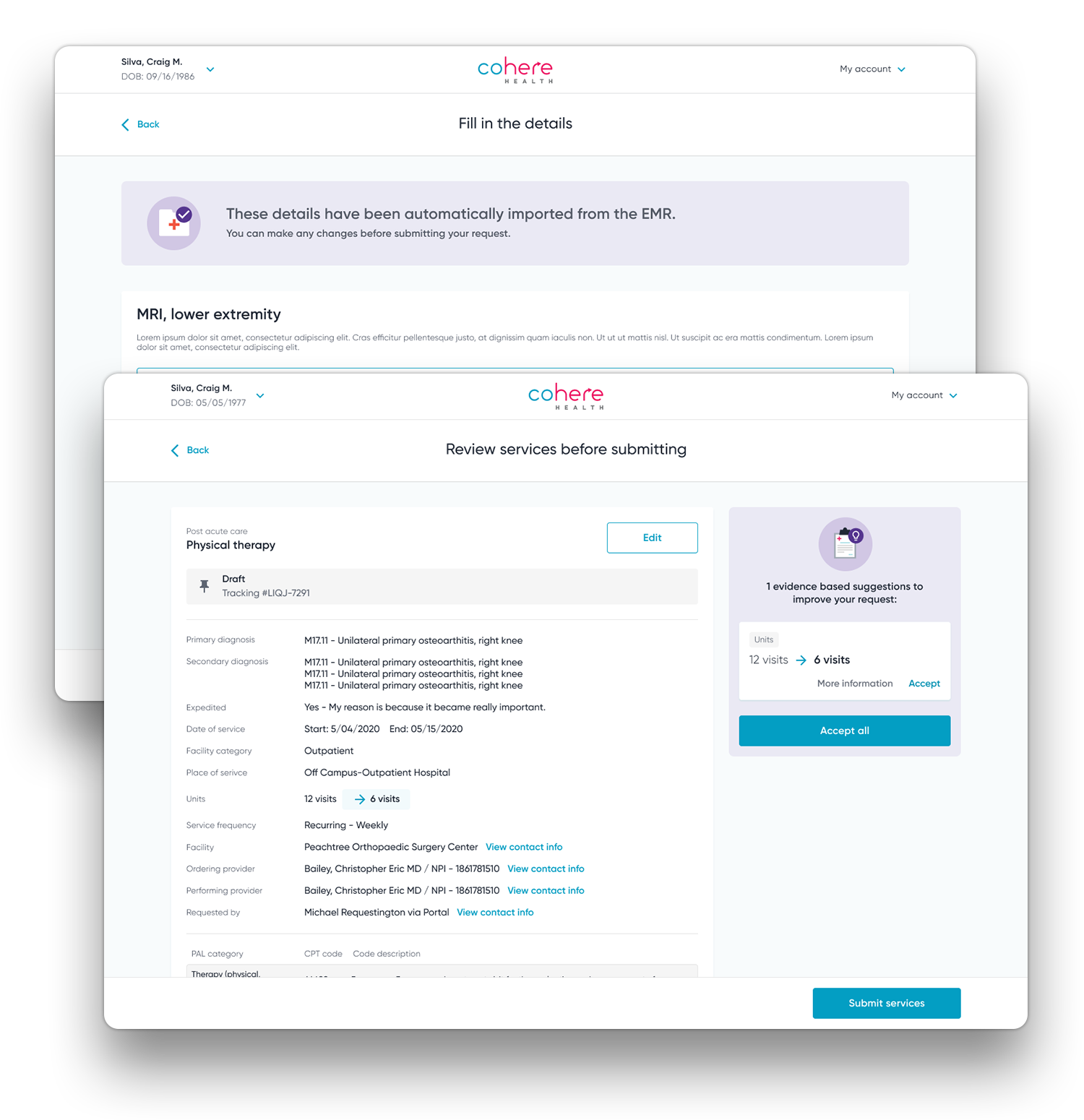
Built on the Cohere Unify™ intelligent prior authorization platform, Cohere Complete™ end-to-end outsourced UM solutions combine deep clinical expertise, AI, and real-time analytics to align health plans, providers, and patients on episode-driven care paths. Our unique approach enables better care quality and outcomes, with fewer denials, and lower medical costs.
We offer fully-delegated, end-to-end management services for key clinical specialties, including:
Physical Therapy
Solutions that shift the focus from individual services to the individual patient
Traditional utilization management programs are about saying “yes” or “no” to individual services, instead of promoting the best patient care and experience. This orientation delays care, and misses an opportunity to proactively drive the best care for that specific patient’s entire care journey.
Proactive, patient-specific care powered by AI
Cohere’s digital-first approach uses interoperability and intelligence to understand the longitudinal patient journey and recommend patient-specific, evidence-based care paths, oriented to the entire care journey. This allows us to help health plans transform utilization management from a reactive, transaction-based program to a proactive one that anticipates optimal care needs for the patient, and guides providers and patients to care choices that improve outcomes and reduce cost.
Solutions that shift the focus from individual services to the individual patient
Traditional utilization management programs, organized around individual services not patients, lead to a patchwork set of systems that are confusing and uncoordinated, causing frustration for providers and patients.
Proactive, patient-specific care
Cohere’s digital-first approach uses interoperability and intelligence to understand the longitudinal patient journey and recommend patient-specific, evidence-based care paths, oriented to the entire care journey. This allows us to help health plans transform utilization management from a reactive, transaction-based program to a proactive one that anticipates optimal care needs for the patient, and guides providers and patients to care choices that improve outcomes and reduce cost.
Our differentiated approach
Robust technology combined with clinical programs, bridge the gap between utilization management and the delivery of quality care.
Patient-specific care plans
Identify diagnostic cohorts and enable the authorization of the entire care episode, rather than a series of individual transactions.
Proactive moments of upstream influence
“Nudge” providers toward patient-specific, clinically optimal care choices and high-value specialists at the point of diagnosis.
Intelligent patient and provider-specific decisioning
Incorporate real-time, provider quality, cost, and care appropriateness insights, as well as patient clinical profile information into the automated determination process.
Clinical analytics
Continuously optimize program performance through advanced clinical analytics including provider benchmarking and performance insights
Watch our recent webinar to understand how our tech-enabled approach has helped drive significant medical cost savings in musculoskeletal for a leading national health plan.

Realize the value of a cutting-edge, digital-first approach