The words “prior authorization” spark nearly universal dread among physicians. Adopting better technologies at the point of intake—including fax digitization, electronic health record (EHR) integration, and portals—makes prior authorization more efficient. Health plans can use these intelligent prior authorization tools to consolidate prior authorization requests across all of these channels into a single digitized workflow, which reduces physician cost and time in the process, and speeds patient access to care, without disrupting workflows.
Fax machines remind me of the scene in Office Space where they destroy the printer. Yet, at least 70% of healthcare practices continue to exchange medical information by fax. Medical practices are one of the only places where fax machines are still common. Why should I enter patient history into a computer, only for my receptionist to print that out and then fax the information? Why can’t it be emailed? This reminds me of going on my computer to MapQuest, and printing out directions to navigate. Now I enter an address in my iPhone and magically receive navigation for the fastest route to my destination. Don’t patients and physicians deserve the same efficiency? Intelligent prior authorization technology can act as an intermediary between the physician and the health plan to create a more efficient care journey for patients by leveraging intake data.
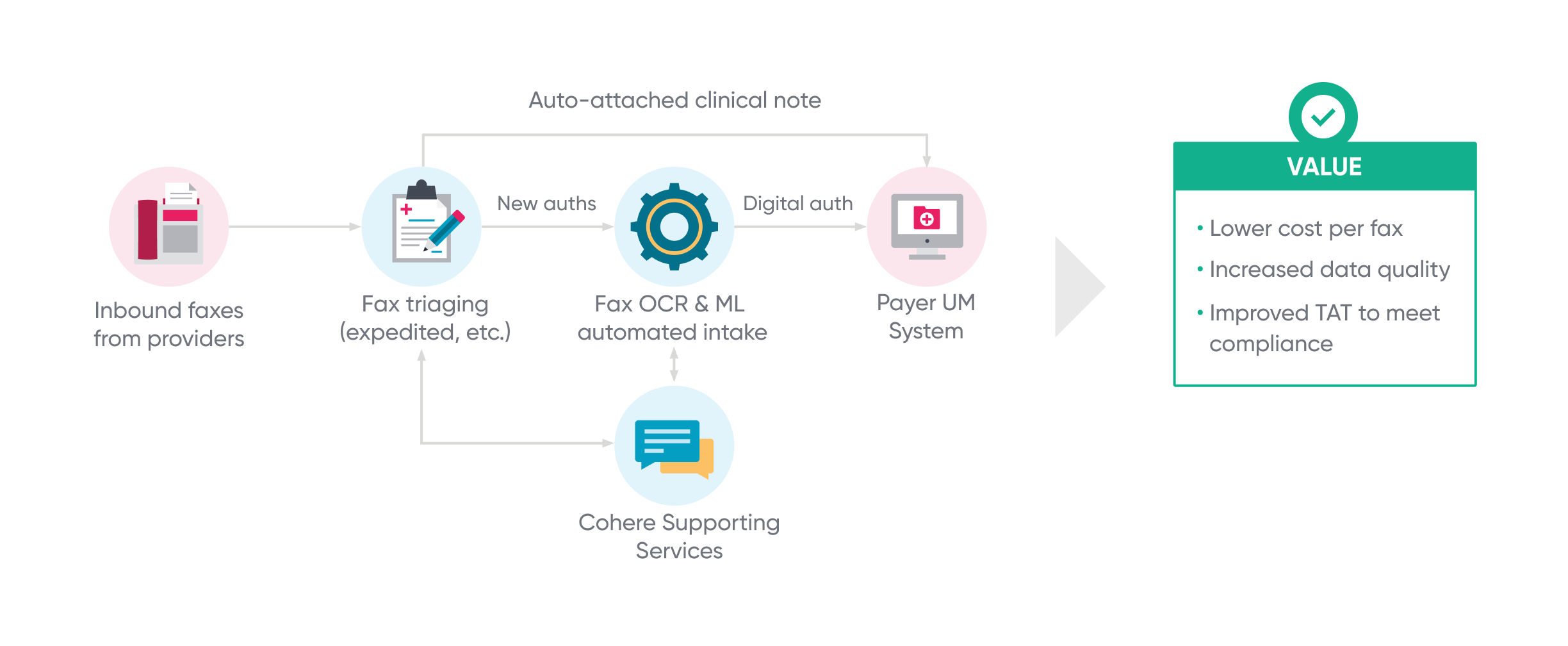
Fax machines offer poor security and tracking. The reliance on fax machines is one reason why prior authorization lags behind most other modern industry processes. Intelligent prior authorization digitizes faxes via optical character recognition (OCR) technology. Faxed data digitized this way can then leverage AI and machine learning to convert physical, printed documents, even handwritten ones, into machine-readable data, that can then “train” intelligent prior authorization technology to look for the most significant data to process the request. This consolidated data can then be combined with data from other intake channels to assist in future requests and reviews. As shown in Figure 1, the resulting workflow presents a lower cost per fax, increased data quality, and improved turnaround time to avoid delays in care and assist in meeting compliance requirements.
Patients and physicians deserve so much better than fax machines. Many health plans are improving collaboration by using a portal as a front door to enable automated authorization requests. High-performing portals report 96% adoption rates by practices, and satisfaction rates soar as high as 92%. Capturing intake data with portal technology streamlines the collection of necessary information in a consolidated, digital format and enables automated decisioning.
EHR integration is another advancement that can revolutionize prior authorization and concurrent review intake. Prior authorization requests do not always contain the information necessary to render a decision, resulting in multiple time-consuming information requests. This leads to delays in care and avoidable peer-to-peer consultations. By integrating directly with a health system’s EHR, health plans can help reduce physician burden and make prior authorization submission nearly invisible. Relevant clinical information can be gathered directly from a patient’s health record to help bolster requests. Automating intake within EHR workflows eliminates non-clinical support staff’s manual efforts, resulting in more complete and accurate submissions to health plans. This morning I did a peer-to-peer call because one important note was missing from the request. If the health plan connected with the EHR, the request could have been approved quicker and with minimal physician abrasion.
Better use of technology at the point of intake is key to unlocking next-generation prior authorization. The ability to leverage health data aggregated from previously siloed intake channels, like fax, portals, and EMR, sets the stage for automated decisioning, improving patient care and decreasing administrative burden.