Automated decisioning is a key capability of intelligent prior authorization, and with a trending regulatory approach to fixing prior authorization supported by a variety of governing bodies, including state and federal bodies, it won’t be long before health plans may be required to implement it. For example, a CMS proposed rule, Advancing Interoperability and Improving Prior Authorization Processes, mandates electronic prior authorization, improved transparency and interoperability measures, and a shortened turnaround time–all of which are supported by automated decisioning. Furthermore, beyond simply automating the authorization decision, intelligent prior authorization solutions use artificial intelligence (AI) to help health plans:
- Improve the accuracy and transparency of decisions
- Reduce the need for peer-to-peer reviews
- Accelerate manual clinical review (when still necessary)
Health plans that implement intelligent prior authorization can enable regulatory compliance while further reducing physician burden & administrative expense, as well as improve care access and quality.
Automated decisioning can be more than just a policy-based, “yes” or “no” decision. Plans can anticipate the entire care episode or journey and proactively suggest care choices that drive better and faster outcomes by applying advanced technology and incorporating analysis of claims and other health plan data. Building off of digitalized intake and EMR integration, intelligent prior authorization solutions can use AI to leverage insights from within the medical record previously locked away in unstructured text. They can suggest alternative treatment plans to improve patient care in accordance with higher quality initiatives, without extra effort from the requesting physician. This allows plans to transcend traditional transaction-centric utilization management and consider a patient’s entire care journey. The short video below shows how a convoluted patient journey can be streamlined if authorization requests are evaluated from the longitudinal perspective of a diagnosis-specific care pathway. Patients receive non-duplicative, cost-effective care sooner and are more likely to achieve positive outcomes.
It’s common for prior authorization requests to be submitted with incorrect or missing attachments. Intelligent prior authorization uses AI to ensure that only complete requests are submitted, which helps to avoid extra work downstream, such as peer-to-peer reviews, denials, and appeals. Consider the pair of images below, which highlight two authorization paths: one manual and one using intelligent prior authorization.
Figure 2: The unhappy path of an authorization
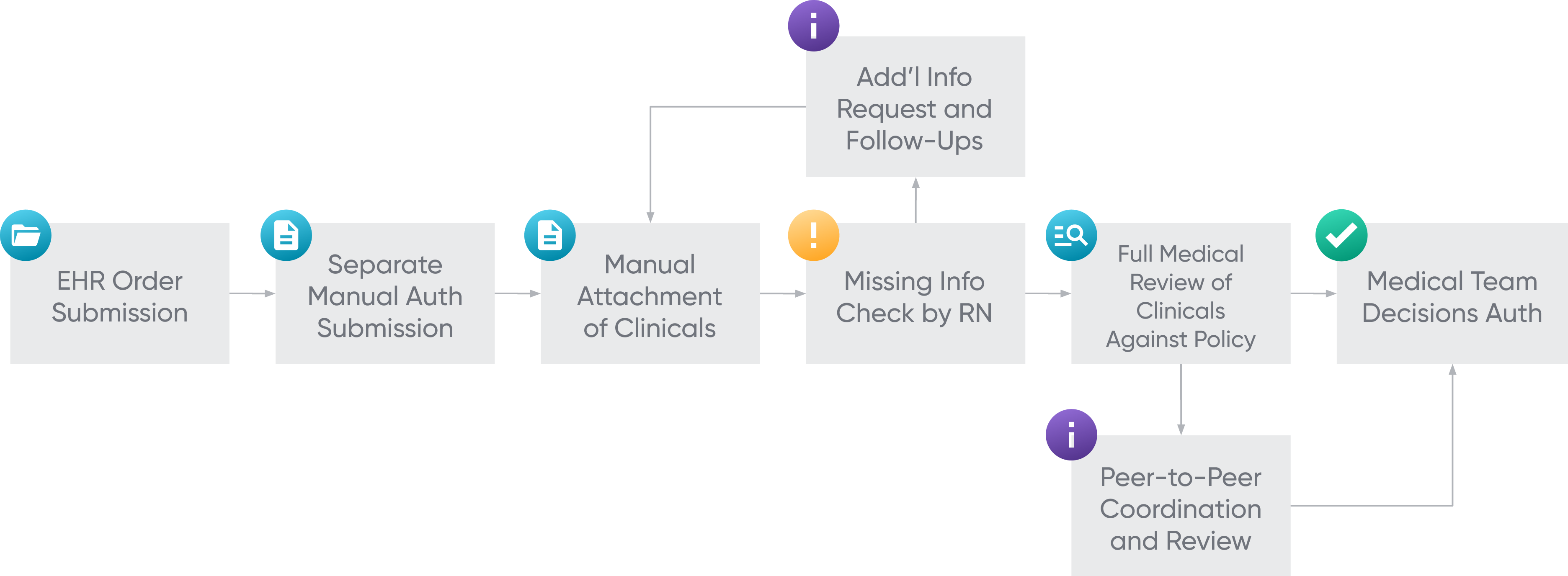
Figure 3: The happy path of an authorization
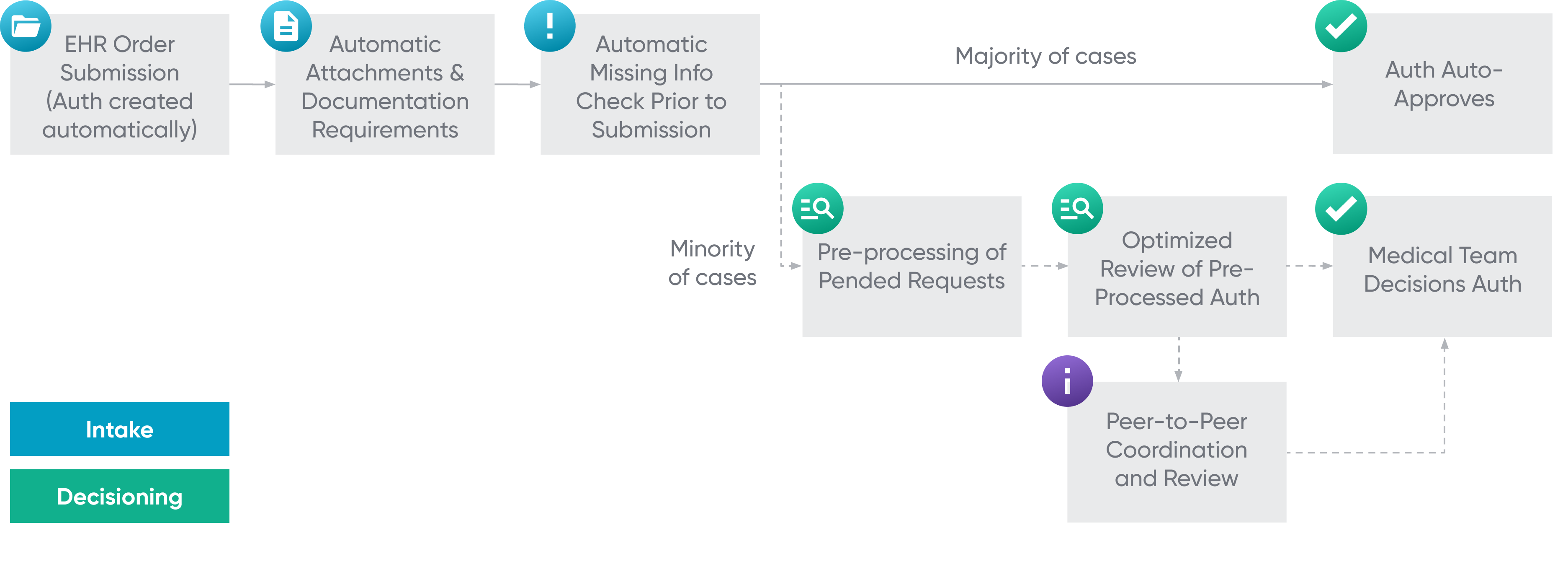
In addition to the completeness scan mentioned above, the diagram also references the pre-processing of pended requests. Intelligent pre-processing capabilities prepare pended cases for review, highlighting relevant pieces of information within clinical documentation and pre-populating clinical reviewer checklists with indications that have been identified by the decisioning engine. This application of AI and machine learning to pull and suggest the most relevant information, so reviewers don’t have to search through pages of disorganized clinical information, improves the turnaround time and accuracy of manually reviewed cases. Pre-processing also enables clinical reviewers to operate at the top of their licenses and reduces the volume of cases requiring peer-to-peer reviews.
The greatest benefit of intelligent prior authorization decisioning is its ability to incorporate analysis of various kinds of data to which health plans have access to improve the accuracy of automated and manual decisioning of prior authorization and concurrent review. By analyzing and applying machine learning to identify the patterns and outliers in approval and denial metrics and claims data, health plans can benefit from greater levels of automated decisioning, while improving decisioning accuracy.
For example, by analyzing provider data for certain services or for certain patient cohorts, health plans can utilize machine learning to help address outlier providers. A few state governments have tried reducing physician burden through gold carding regulations, which consider providers’ authorization history for certain services and, if it meets a certain percentage approval threshold, exempt them from authorization requirements for those services going forward.
Gold carding legislation efforts are well-intentioned, but they leave health plans and patients exposed to increased healthcare costs and patient risk. In a recent survey conducted by AHIP, 73% of health plans with gold carding programs reported some negative outcomes, such as administratively difficult implementation, higher costs, and reduced quality of care for patients. The survey, which included health plans with discontinued gold carding programs, also stated that 75% of plans cited “administratively difficult implementation” as the most common reason for discontinuation of the programs. Health plans require advanced solutions to provide them with the technological scaffolding to comply with legislation and transform utilization management.
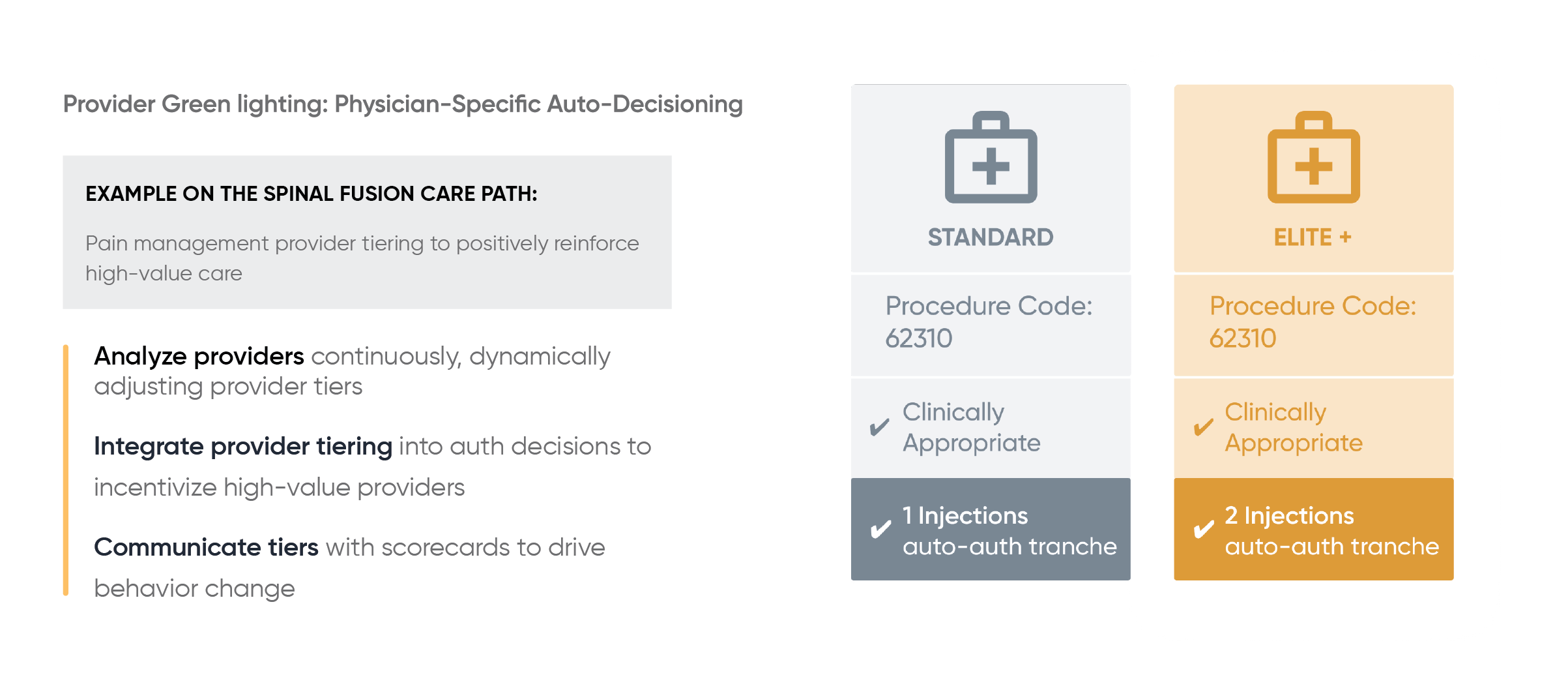
Pioneers in the intelligent prior authorization space have developed a more comprehensive alternative to gold carding, called green lighting. Green lighting refines the technique behind gold carding efforts to ease and enhance the quality of implementation. Instead of relying on historical, thereby stagnant, data, green lighting uses real-time analytics to identify providers that meet certain quality criteria, or even whole practices, and simplify their authorization process. Green lighting incorporates patient data in these evaluations, so physician results are diagnosis-specific. In this way, health plans can comply with new regulations for gold carding, isolating green lighting to specific in-scope services for the physicians who get routine approval for them, without compromising the decisioning and delivery of evidence-based, quality care. Green lighting also makes it possible for health plans to identify and work with underperforming practices and physicians to increase transparency around decisioning and enhance care. The image below illustrates an example of how green lighting works within a spinal fusion care path. See how green lighting streamlines the process of complying with regulations while maintaining medical expense impact.
The most impactful opportunity for health plans considering automation would be the implementation of an intelligent prior authorization solution that goes beyond simple automation of decisioning along policy guidelines, and instead uses advanced technology to incorporate different forms of data to enhance decisioning capabilities beyond the policy. Health plans have a huge opportunity to improve utilization review if they consider compliance with changing regulations as a catalyst for transformation.
For more information about the benefits of intelligent prior authorization, download our white paper.