A recap of Cohere’s latest webinar with ACAP
Following the announcement of the new CMS proposed rule on prior authorization, Cohere Health and ACAP (the Association for Community Affiliated Plans) hosted a timely Q&A to answer the most pressing questions we’ve been hearing from health plans about complying with the upcoming regulatory changes. Our expert panel featured: Alina Czekai, VP, Strategic Partnerships; Adrian Thomas, M.D., Associate Medical Director; Sam Stearns, VP, Payer Solutions; and myself.

If you missed the live session, please read the recap of our insights and answers below.
The webinar is now available to watch on demand. Tune in to get all of the intel on the forthcoming changes and how health plans can start preparing today.
Background: Understanding the CMS proposed rule
The call for prior authorization reform is everywhere. And for good reason. In an eye-opening American Medical Association report, 93% of physicians surveyed reported care delays associated with prior authorization, while 91% reported that authorizations negatively impacted their patients’ clinical outcomes. Among my fellow physicians, and for health plans and patients alike, there has been a steadily growing recognition of the need to improve prior authorization for all parties involved.
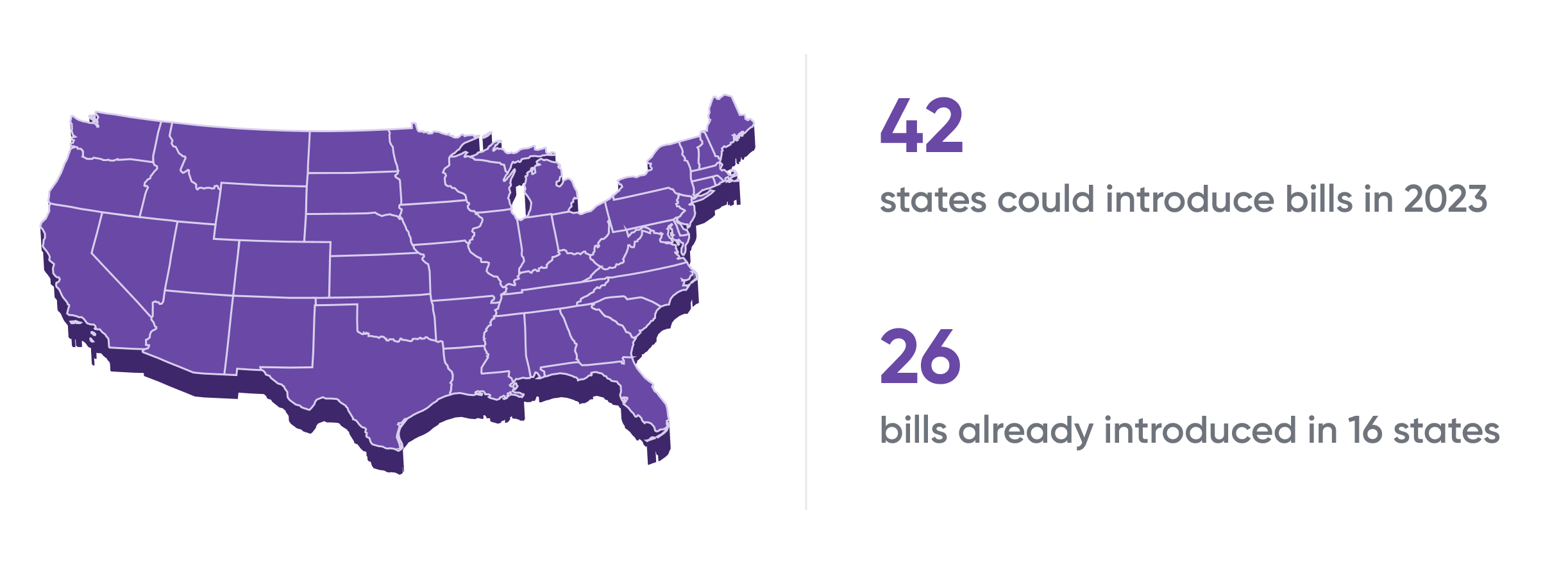
Numerous states, including Michigan and Texas, have already enacted legislation to address the ongoing issues with prior authorization, including physician gold carding policies, faster turnaround times, and more. Per AHIP, there were already 26 bills introduced in 16 states as of mid-January, with the expectation that we will see bills aiming to improve prior authorization proposed in 42 of 50 states in 2023.
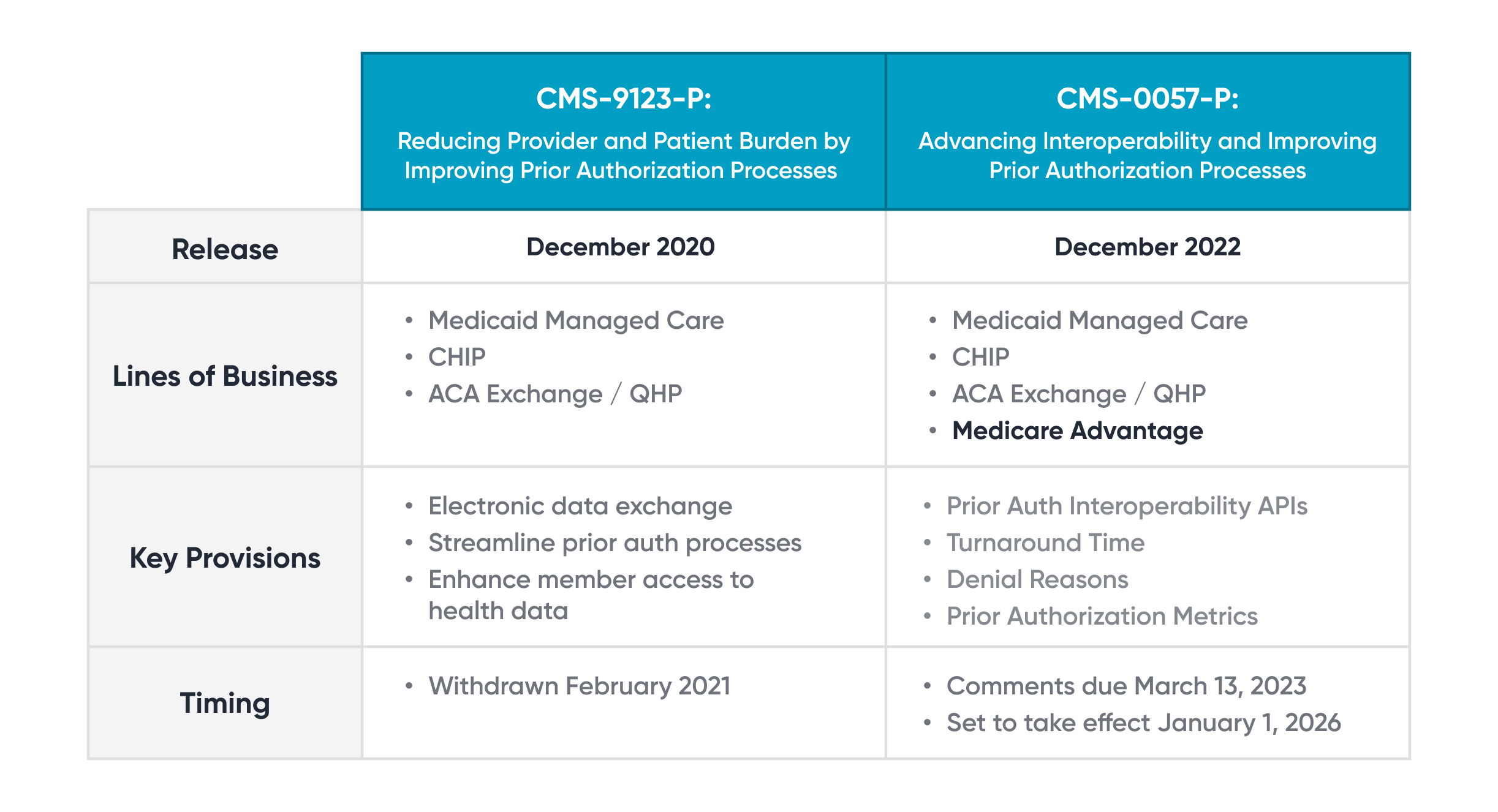
Now, the federal government is also responding to the growing calls for reform. In December 2022, the Centers for Medicare & Medicaid Services (CMS) proposed a new rule (CMS-0057-P) with the goal of advancing interoperability and improving prior authorization for Medicare and Medicaid patients. This isn’t the first time federal legislation has been introduced to improve prior authorization. A rule to reduce provider and patient burden by improving prior authorization (CMS-9123-P) was proposed in December 2020 but later withdrawn. The increasingly widespread appetite for change is clear.
The new rule, Advancing Interoperability and Improving Prior Authorization Processes, includes new lines of business and five main provisions; it is scheduled to take effect on January 1, 2026. In this webinar, my colleagues and I helped the audience take a closer look specifically at the Improving Prior Authorization Processes provision and its four key policies:
FAQ: Health plans’ top questions on the prior authorization provisions
At Cohere, we believe these changes can achieve greater transparency for patients, physicians, and health plans; reduce physician burden and friction; and, most importantly, ensure our patients get the right care at the right time.
As a pioneering force in prior authorization technology and transformation, Cohere has been fielding countless questions from health plans across the country who are looking to:
- Make sense of the new rule (403 pages – yikes!) and how it will impact their operations, and
- Get ahead with a strong compliance strategy before the rule goes into effect.
We are eager to answer the big questions and help our current and future partners prepare for the transition to a new regulatory environment.
Interoperability
Q: How will the application programming interface (API) standards help health plans transition toward compliance?
A: The purpose of the APIs and setting standards for them is to ensure patients, physicians, and health plans can all access the appropriate level of information. This is critical for a physician trying to make care decisions or a patient wanting to understand their care journey. These standards will help all of us involved in a patient’s care be able to “talk” to one another with technology (which also further supports compliance with the rule’s transparency guidelines). When everyone involved in a patient’s care communicates, patients can experience better outcomes.
Turnaround times
Q: What strategies are health plans pursuing to improve their turnaround times (TAT)?
A: As health plans prepare for much faster required turnaround times for authorization decisions, the most forward-thinking plans are investing in technology solutions to digitize and automate their prior authorization processes. When health plans are able to automatically approve clinically appropriate cases, our patients get the care they need faster and, consequently, experience better health outcomes.
Transparency
Q: How will transparency guidelines impact patients, physicians, and health plans?
A: As it stands today, it feels like my fellow physicians and I are playing a board game, but we haven’t been told the rules. Healthcare isn’t a game. These are patients’ lives. And if physicians aren’t told the rules, our patients lose.
These guidelines will require health plans to communicate their requirements and denial reasons to physicians; that way, we can ensure all criteria are met before submitting an authorization. Greater transparency can speed up access to care, decrease the longstanding friction between physicians and payers, and improve the patient and physician experience.
Accountability
Q: How can I be more accountable to the metrics I need to publish?
A: Accountability is critical in its own right, but it’s made possible by transparency. More transparency leads to better accountability: health plans can compare themselves to their counterparts and ensure they meet best practices.
As value-based care becomes more prominent, health plans should be part of the value equation. Accountability is an important step to ensuring physicians and health plans get insight into how they can continually improve and drive higher-value care.
What next? How health plans can prepare
As a health plan, there is much to unpack about the proposed rule and how to address all that needs to change before the final version goes into effect in January 2026. This will be a transition period, especially for those plans at the beginning of prior authorization transformation, but we are optimistic about the positive impact these changes will have on patients, physicians, and health plans. The question is: how can health plans prepare for compliance with the forthcoming changes?
The answer: Cohere can help. Whether your plan is looking to get started on interoperability (we’re already supporting numerous Fast Healthcare Interoperability Resources [FHIR] APIs in production) or transparency (we publish transparent care path guidelines), our intelligent prior authorization solutions are helping innovative health plans across the country: transform their prior authorization processes; provide better care and outcomes; improve physician experience and ease administrative burden; and get ahead of compliance before 2026.
Now is the time to address your compliance game plan. What are you doing to get started?

