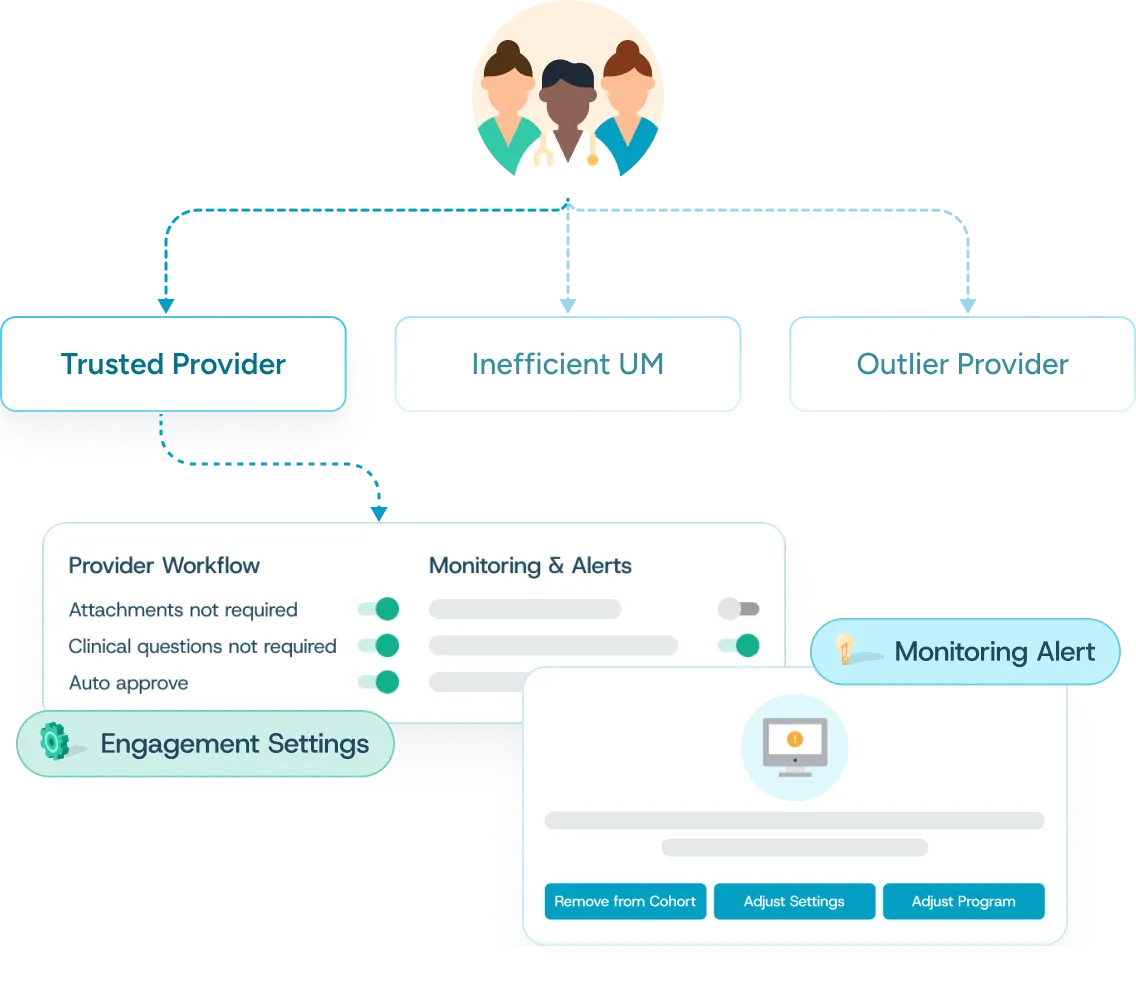
Achieve more than gold carding
Personalize the provider experience to streamline, improve, and save.
Unlike traditional gold carding programs that bypass PA measures entirely, Cohere Align™ delivers control and security, with finely tuned monitoring to understand changes in provider behavior, reduce risk, and optimize accordingly. Proven to improve provider satisfaction by configuring the approval path to meet their needs, Cohere Align can be a central component of your provider network strategy. Cohere Align’s advanced analytics and curated provider touchpoints enable you to deliver tailored PA experiences that:
- Streamline. Reduce administrative burden and provider abrasion.
- Improve. Drive clinically appropriate authorizations.
- Save. Improve efficiency and reduce manual reviews to achieve savings.