A recap of Cohere’s latest webinar with Humana
HealthPayerIntelligence kicked off 2023 with a highly anticipated webinar featuring Cohere and Humana leadership. Our expert panel included Brian Covino, M.D., FAAOS, Chief Medical Officer, Cohere Health; Gina Kim, Chief Product Officer, Cohere Health; and Lisa Stephens, MBA, PMP, Senior Vice President of Operations, Humana.
If you missed the live session, unpack the key insights in this brief recap.
The webinar is now available to watch on demand. Tune in to learn about Cohere and Humana’s continued partnership and our journey to transform prior authorization.
The background: Humana & Cohere
Always at the forefront of innovation and utmost quality care, Humana wanted to transform their prior authorization operations to trigger better care and better experiences for everyone involved in and touched by the authorization process. As Lisa shared during our conversation, members with poor prior authorization experiences are 10% more likely to disenroll from their plans, despite the best efforts of their plan and provider to get them the right care at the right time. Furthermore, provider surveys showed that prior authorization was consistently a leading pain point for those delivering care.
Humana knew something had to be done about the provider abrasion borne out of traditional prior authorization practices. They needed to foster better, more streamlined collaboration with providers in the context of their members’ care journeys.
The goal? Leverage intelligence and automation to innovate at scale and, ultimately, decrease provider abrasion and improve the health and outcomes of their members. Humana sought to address this by:
- Removing unnecessary steps and low-value, wasteful care
- Starting with areas of large spend, such as musculoskeletal (MSK) and cardiology care
- Aligning providers and health plans on high-quality, high-value care paths
- Bringing the process upstream with earlier, more proactive interventions
The transaction to transformation continuum
Dr. Covino explained how health plans across the country are all at some stage in the process of transforming their authorization processes. Whether health plans are motivated by forthcoming regulatory requirements or wanting to reduce outcomes variations and cost, there is an appetite for change.
Some plans are starting toward the bottom of the pyramid below. These plans are seeking foundational things, like complying with regulations, or shifting away from manual, time-consuming processes like the dreaded fax. Plans at the middle of the pyramid are at the utilization impact stage, wherein new tech like AI/machine learning can help drive clinical choices beyond just the authorization request. Examples include suggesting a different, more appropriate site of service for a given member.
 The top of the pyramid is where we find the most forward-thinking plans, like Humana, who are using prior authorization as a launching point for a more longitudinal care approach. This type of plan thinks beyond individual authorization transactions – they consider the whole patient journey. That may manifest as suggesting care paths for specific patient situations, or combining and approving multiple authorization requests for an entire episode of care up front.
The top of the pyramid is where we find the most forward-thinking plans, like Humana, who are using prior authorization as a launching point for a more longitudinal care approach. This type of plan thinks beyond individual authorization transactions – they consider the whole patient journey. That may manifest as suggesting care paths for specific patient situations, or combining and approving multiple authorization requests for an entire episode of care up front.
At this level, innovative health plans can effectively help their members achieve the best and fastest care and outcomes, beyond simply saying “yes” or “no” to individual authorization requests.
Results
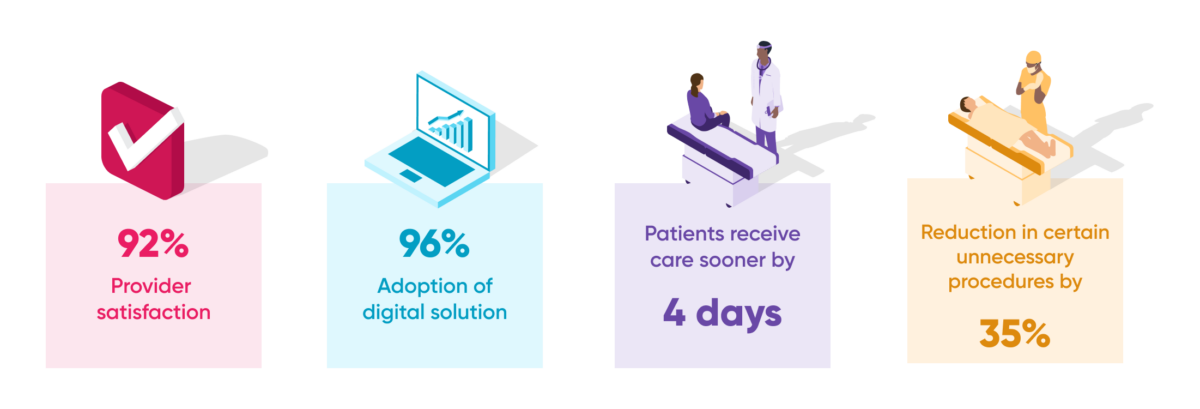
As a result of this transformative new approach to prior authorization, Cohere and Humana are driving prominent and unique impact for both members and providers. Take a look at some of the results we explore in the webinar:
How does prior authorization innovation drive value?
Humana aimed to harness intelligence and automation to innovate at scale, but how does this innovation drive unique value? Beyond enabling a longitudinal approach to members’ care journeys, Humana’s approach meets providers where they are and unifies a historically siloed experience.
Gina explains that one of the most effective strategies for meeting providers where they are is by creating a single digital “front door” to the health plan across all prior authorization channels. In addition to replacing multiple input processes with just one, this approach establishes a foundation from which to drive intelligent guidance into providers’ workflows, so they can make care choices more likely to drive better patient experience and outcomes.
- Automate: We’re able to automate traditionally manual, burdensome processes (think faxes and phone tag) to reduce processing time and cost for both providers and health plans.
- Integrate: We integrate into the provider’s EMR, where much of the data needed to submit authorizations already lives – this is central to meeting providers in their current workflows.
- Portal: Consolidating authorization activities within providers’ existing web portals makes it easier and faster to process requests and ultimately creates a unified, consistent experience.
Unifying the provider experience enables a plan to leverage clinical intelligence within the provider authorization workflow; this is where Cohere brings significant analytics expertise and enables the right decisions to be made on a granular level. This approach utilizes all data available as a member progresses through their journey; building a patient profile via clinical notes, claims, SDoH, and other key data helps make better care decisions. Learn more about this new approach to driving value at scale.
What comes next
Moving forward in the current environment, plans need to find a way to traverse ongoing provider abrasion, abundant regulatory changes, and rapid advances in available healthcare tech. Humana and other forward-thinking health plans are taking a thoughtful two-pronged approach to transformation.
By harnessing industry collaboration and innovation at scale, Humana and other leading innovators can unlock meaningful value across four key areas:
- Differentiated capabilities
- Cost of care
- Member experience
- Member outcomes
Furthermore, CMS’ newly proposed rule (CMS-0057-P) is making headlines. Medicare and Medicaid plans are now facing additional regulatory challenges vis-à-vis electronic prior authorization requirements and must be prepared to comply by January 2026. Learn how to get ahead of these legislative changes in our recent webinar with ACAP and Cohere’s compliance experts.
Final thoughts
As the panel wrapped up, Lisa added that Humana’s “strategic bet right now is on Cohere. I consider them a thought partner and strategic leader in the industry, and we are excited about the work ahead.”
Stay tuned for what comes next in this ongoing partnership at the forefront of prior authorization transformation.

