Physicians Deserve a Better Peer-to-Peer Experience
Published:
August 12, 2022

Peer-to-peers: A physician’s day in the life
I read a message in my inbox: “The prior authorization for Jane Doe’s MRI went to peer-to-peer review.” I groan. How and when am I going to fit this in? I already have 30 patients on my schedule. Between seeing patients, reviewing labs, answering patient messages, and processing refills, I already missed lunch; I decide I’ll do the peer-to-peer later.
The next day, my office manager reminds me, “You really need to do that peer-to-peer.” I finish with my last morning patient and make the call, but shortly after I’m placed on hold. In between bites of my lunch, I spend twenty-six minutes on countless holds and repetitive back and forths with the insurance company, before I’m finally connected to the physician for the patient’s peer-to-peer (P2P) review:
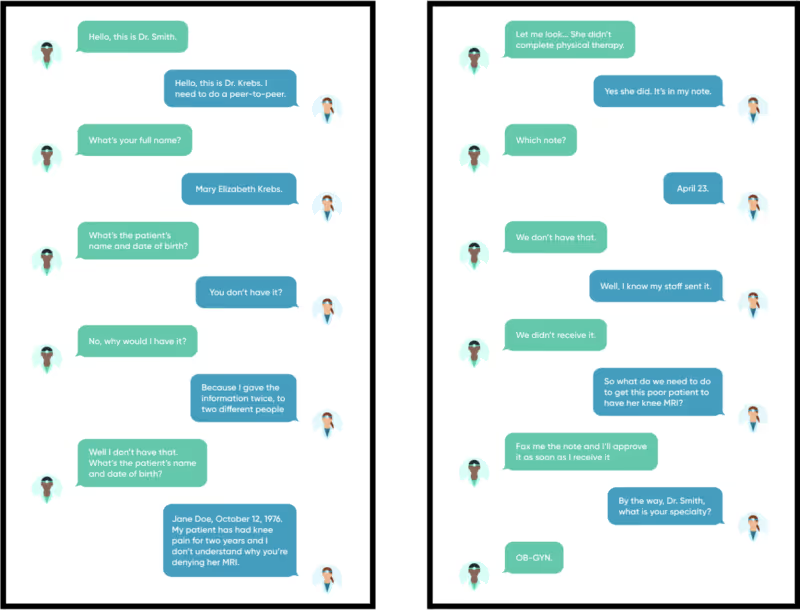
Peer-to-peer reviews are intended to offer transparency into the prior authorization process; to ensure all physicians are following evidence-based clinical guidelines. In practice, however, the process has become inefficient, abrasive, and at times even detrimental to our patients’ experiences and outcomes.
How does the peer-to-peer process impact physicians – and our patients?
Our country is experiencing a physician shortage on top of widespread burnout among healthcare workers, and the inefficiencies of the peer-to-peer process only exacerbate the shortage and burnout crisis. It’s imperative that we start implementing solutions that, rather than making important healthcare decisions nearly in a vacuum, take into account – and actively support – physicians’ workflows so that they can focus wholeheartedly on patient care.
The process wastes so much time between call-waiting or speaking to a physician of a different specialty who may not have reviewed the case, and sometimes occurs only because of miscommunication. Beyond the physician abrasion exacerbated by the peer-to-peer review process, it can also be harmful to our patients. Earlier this year, an insurer denied a North Carolina patient’s MRI that she desperately needed. When she finally got the MRI over a month later, it revealed cancer, and she later died. This delay in care is unacceptable, and her death is heartbreaking and infuriating. The peer-to-peer process is at best frustrating and burdensome, and at worst can cause real delays that negatively affect our patients’ care.
We need to improve peer-to-peers, to ensure patients receive the care we know they need in a timely, efficient manner. As a physician, the prior authorization process can feel like we’re back in second grade, when the entire class lost recess because one or two kids misbehaved, simply because a few physicians or nurse practitioners may have ordered a test without necessary documentation. It’s time to rethink the process for those consistently providing high-quality care; to allow them to focus their time on caring for patients.
Creating a better way forward
One of the reasons I joined Cohere Health is to improve prior authorizations and other hassles physicians go through – like peer-to-peer reviews – so that they can spend their time actually helping patients. I love the approach: we assume physicians are trying to get the best care for their patients while managing a demanding job, and we actively look for ways to better support them. Some of the ways we do this:
- Intelligent automation: As mentioned in a previous paper on how we’re transforming utilization management (UM) with artificial intelligence and machine learning, Cohere’s platform auto-approves clinically optimal requests in almost 90% of cases, resulting in 63% lower denial rates, fewer cases necessitating review, and thus fewer delays. Instead of adding friction and wasted time, we help physicians optimize care and the time they’re able to spend with each patient, improving physician and patient experiences alike.
- More valuable peer-to-peers: Cohere strives to ensure that only a minimum of cases even get to the peer-to-peer stage. We make multiple attempts to make sure we have all the information, so we prevent unnecessary peer-to-peers, like the one I described. We schedule the peer-to-peer and call the physician or nurse practitioner at the number they prefer, which avoids long holds and a painful phone loop. Our peer-to-peer reviews are actually with physicians of the same speciality who have reviewed the case before the call.
- Physician-led: Our founders and board include a number of physicians with experience in both practice and leading healthcare companies. I also get to work alongside teams of esteemed physicians who help shape the platform and ensure that physicians’ needs and workflows are central to decisions about our solutions.
Cohere Health helps to ease the burden placed on physicians by traditionally labor-intensive prior authorization systems and to improve their experience, all with the goal of delivering the highest quality care to our patients.
To learn more about the work we’re doing to improve physician and patient experiences during the prior authorization process, download our whitepaper on digitally reinventing UM or our case study for KLAS’ Payer/Provider collaboration initiative.
Available For Download
Written by

Mary
Krebs, M.D., FAAFP
Dr. Krebs serves as the Medical Director of Primary Care at Cohere Health. She earned her medical degree from the Ohio State University College of Medicine in Columbus and completed a family medicine residency at Miami Valley Hospital in Dayton, Ohio. She also teaches residents and medical students at a family medicine residency program. Previously, Dr. Krebs was in solo practice at a rural federally-qualified health center and co-ran Family Practice Associates, an independent rural practice.
Stay ahead with expert insights on transforming utilization management and payment integrity—delivered straight to your inbox.


