Health plans are looking to intelligent prior authorization to improve the efficiency of their workflows, save on administrative costs, and enhance the provider and patient experience. As a physician, I’m excited by the attention that reforming prior authorization has garnered and intrigued by the recent conversation about using responsible artificial intelligence (AI) in healthcare. While prior authorization is an essential process, there are many ways to use innovative technologies to make the process more efficient and less burdensome for us and our staff.
Since physicians and their staff spend an average of two business days per week on prior authorization, improving the process will go a long way in reducing the friction between health plans and physicians. Health plans implementing intelligent prior authorization are best situated to improve the health plan-physician relationship because it reduces administrative burden and applies clinical intelligence to improve patient outcomes. It helps health plans leverage the service request transaction to shift provider network relationships from tense to collaborative using responsible AI.
Here are some of the most common questions we hear from health plans concerned about physician experience
Q: How does implementing a portal impact provider experience?
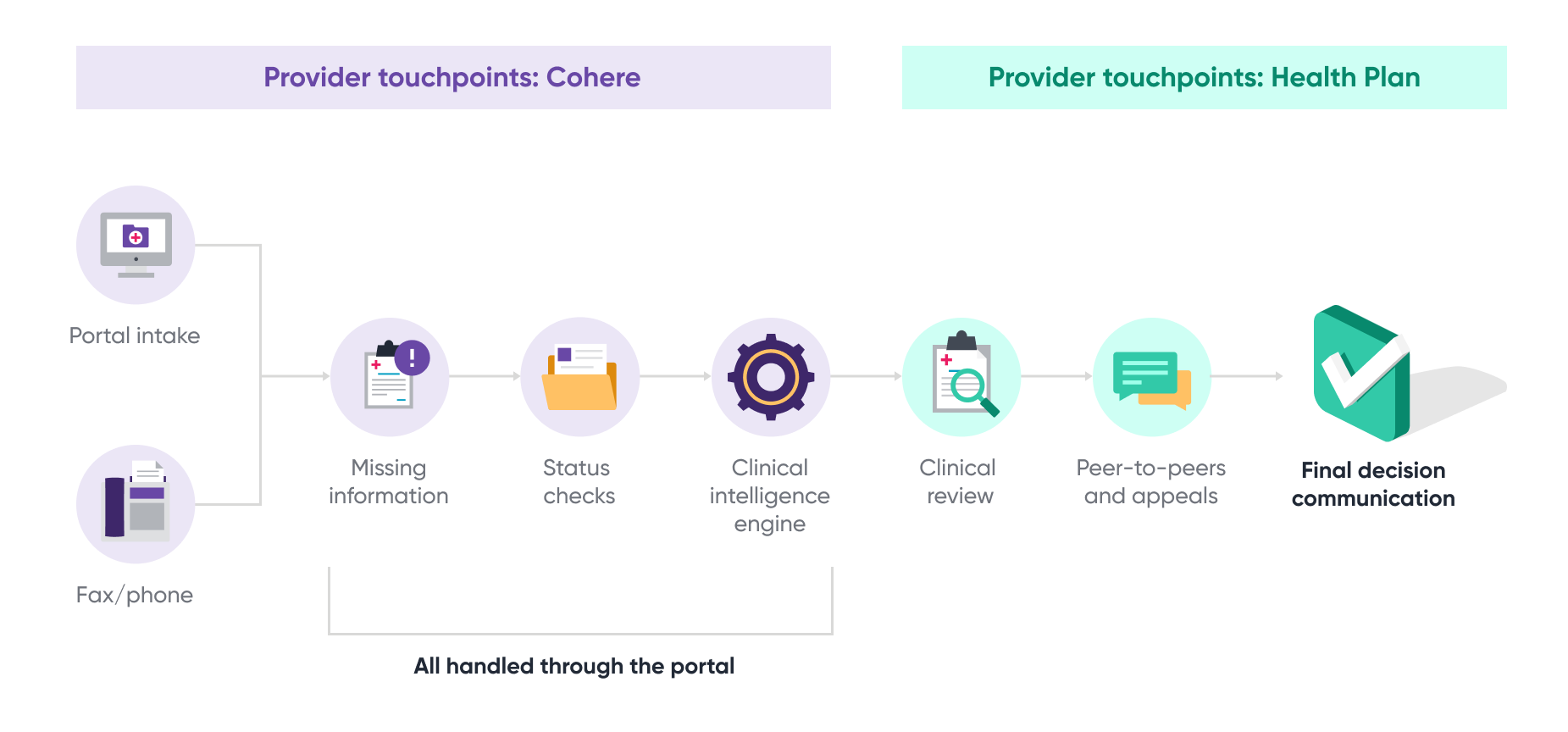
A: A portal-based prior authorization solution increases efficiencies and reduces physician time, costs and effort, when compared to manual processes, such as fax. Physicians submitting authorizations via portal can directly log into the Cohere portal, or can log in from the health plan’s portal via single sign-on (SSO) technology.
There are some additional benefits to submitting authorizations electronically. Physicians can transparently see which services require authorizations and what clinical documentation is needed to determine medical necessity. Feedback is mostly instantaneous-in many cases, the request can be approved immediately in real time. For cases that must pend for manual review, physicians can check on the status of their requests online, without waiting for communication from plan staff.
Q: Communication can be a major cause of friction between physicians and health plans. What is the notification process for authorization status, need for additional information, or denials?
A: There are three methods to communicate our determinations to patients and physicians. Depending on how the physician sent in their service request, we will notify them of a decision via:
- Portal (instantaneous)
- Email (if provided)
- Mail, fax, or phone (as a last resort)
Cohere follows CMS protocols for decision notification. As a best practice, we also follow CMS protocols for commercial lines of business.
Q: Does intelligent prior authorization use AI to deny authorization requests?
A: The Cohere platform does not use AI to deny authorizations. Ever.
Cohere leverages health plans’ specific policies, along with national policies, such as NCD/LCD, in order to approve requests, or pend requests for review by a credentialed clinician. That way, standards of care are applied consistently across a plan’s entire membership in the authorization process.
For all cases that cannot be auto-approved, clinical experts review the request and make any final judgment concerning denial to ensure clinical accuracy.
Q: Automated clinical review sounds too good to be true. How does intelligent prior authorization validate prior authorization requirements for members and providers?
A: The Cohere platform uses AI and machine learning to conduct automated, real-time checks for prior authorization requirements based on the member’s specific coverage and the health plan’s prior authorization requirements. This functionality is supported by integrating the health plan’s benefit and network information. This information is used to configure rules logic to ensure coverage for appropriate services and identify in and out-of-network providers for the patient.
Q: Regarding gold carding alternatives, such as green lighting, what is the volume of authorization requests required for physician eligibility?
A: To streamline the prior authorization process and reduce physician burden, we want to green light as many physicians as we can, while maintaining accuracy standards. While low-volume physicians are not currently eligible for green lighting, high-volume physicians, such as arthroplasty surgeons, may be eligible for green lighting.
Q: Is green lighting performed at the provider level? Or for specific procedures?
Of plans that implemented gold carding programs, 73% reported some negative outcomes, such as administratively difficult implementation, higher costs, and reduced quality of care for patients. Green lighting uses real-time analytics to determine if providers, provider groups, or even facilities, are meeting specific approval thresholds for a given service. This eases the implementation and administrative burden seen with gold carding programs, while still meeting gold carding regulatory requirements.
Q: Do providers know they are being green lighted?
Cohere delivers provider scorecards which can be used by health plans to educate physicians on approval criteria and best practices to achieve or maintain green lighting status. Notifications keep physicians informed of the criteria for different services and their status.
Cohere reduces the physician burden of prior authorization with its user-friendly workflow automation
Physicians and their administrators are immensely satisfied with their experience using Cohere. Our satisfaction rate is 90%, and we have a provider net promoter score (NPS) of 61 across all specialties.
As one respondent put it, “Cohere is, hands down, the easiest authorization process/system I use on a daily basis.”
Learn more about how intelligent prior authorization could transform your prior authorization process.